1- SENSING
A properly functioning defibrillator is capable of sensing rapid, low-amplitude signals, during ventricular fibrillation (VF), without sensing the T wave or extracardiac signals during sinus rhythm. This implies the programming of a high sensitivity and short refractory periods. The sensing threshold, instead of being set at a fixed value as in a cardiac pacemaker, is automatically adapted as a function of the preceding R wave’s amplitude. The detection circuit is blind during the blanking period, which is programmed at a short value to prevent multiple detection of the same depolarisation, while maintaining the ability of detecting very fast tachycardia. At the end of the blanking period, the adaptation of the sensitivity begins at a percentage of the sensed R wave’s amplitude, before gradually decreasing to the lowest programmed value. Each manufacturer has chosen specific values of a) baseline sensitivity from the time the R wave was sensed, and b) the rate of rise of the sensitivity during the cycle. The nominal minimum sensing is 0.8 mV, and the blanking period (absolute post-ventricular sensing ventricular refractory period) is 110 ms in the latest defibrillators and 80 ms in the earlier models. These values allow a proper detection of VF in the majority of patients when the R wave amplitude during sinus rhythm is >5 mV. The programmed refractory period and minimum sensitivity can be validated during the induction of VF, enabling its flawless detection, while avoiding oversensing of the T wave or any other extracardiac signal.
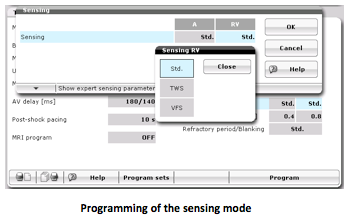
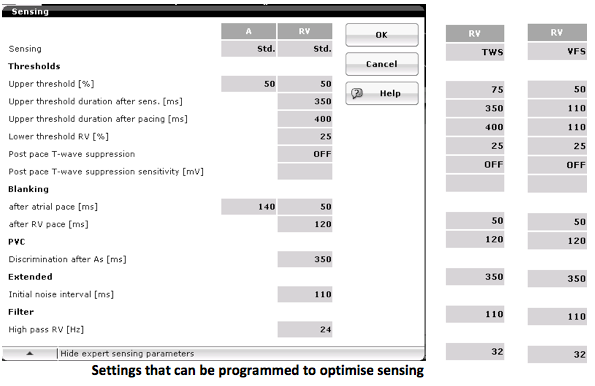
SelectSense function
A choice of 3 settings is available to control the sensing function and analysis of the right ventricular EGM:
- standard programming (Std)
- enhanced T wave suppression (TWS)
- enhanced VF sensitivity (VFS)
In Biotronik defibrillators older than the Lumax 740, the bandwidth ranged between 24 and 60 Hz. Since the 740 model, the bandwidth has been widened to between 24 and 100 Hz.
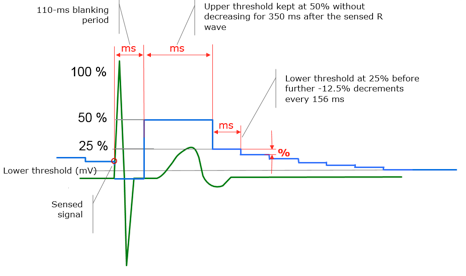
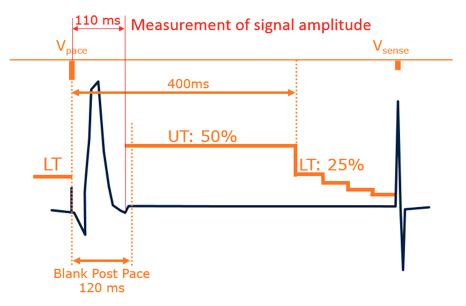
Standar programming
The analysis of a ventricular EGM includes a positive and a negative component. Biotronik defibrillators measure the amplitude of the highest positive or negative peak. The onset of an R wave is followed by a 110-ms blanking period, after which ventricular sensing begins for amplitudes >50% of the sensed R wave (upper threshold at 50%). This threshold persists for 350 ms (360 ms for defibrillators older than the 740 model) after sensing of the R wave (240 ms after the end of the blanking period). Thereafter, the sensitivity increases to a 25% threshold (25% lower threshold) for a 156-ms duration. In the Lumax 740 defibrillators, the sensitivity increases regularly throughout the cardiac cycle in further decremental steps of -12.5% every 156 ms until it reaches either the nominal sensitivity of 0.8 mV, or a value programmable between 0.5 and 2.5 mV. In older models, the steps were 0.125 mV every 156 ms.
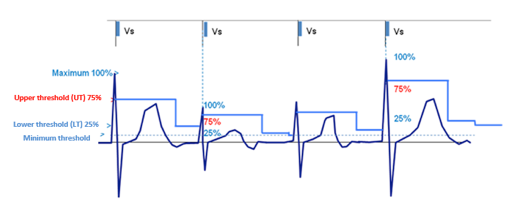
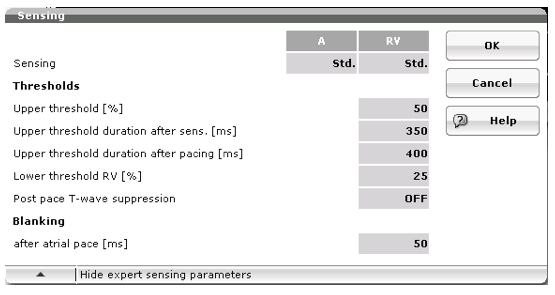
SEnhanced T wave suppression
This programming, designed to prevent T wave oversensing by decreasing the defibrillator’s sensitivity in the beginning of the cardiac cycle, modifies 2 settings: 1) the upper threshold is increased to 75% of the R wave amplitude (instead of 50% in the case of standard programming) for a 350-ms period, while the lower threshold is at 25%; 2) the filters are modified to prevent the amplification and sensing of the T wave: the high-pass filter is increased to 32 Hz (24 Hz in the case of standard programming). This programming is discouraged when the quality of sensing is low or medium.
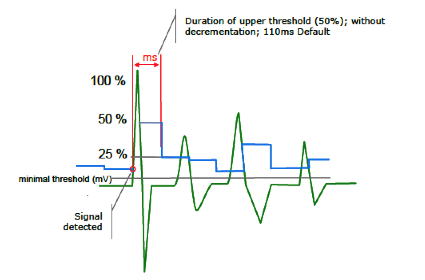
Programming of enhanced VF sensitivity
This programming sensitizes the defibrillator to prevent undersensing of the R wave. This is achieved by maintaining the upper threshold at 50% of the R wave amplitude for 110 ms. In older device models, the blanking period lasted 80 ms, such that the the upper threshold was maintained at 50% for 30 ms, while the lower threshold was at 25% of the R wave amplitude. In the newer models, sensing begins directly at 25% of the R wave, at the end of the 110 ms blanking period. The high-pass filter is also increased to 32 Hz to prevent oversensing of the T wave. This setting should not be used if the T wave is oversensed.
Supplemental settings
Some settings can be programmed independently and individually to optimise the quality of ventricular sensing. However, the access to these settings is protected by a code known only by the employees of Biotronik Inc.
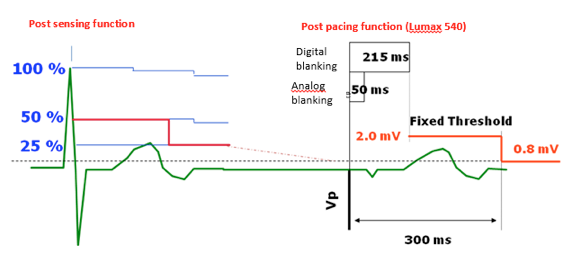
Sandar sensing after ventricular pacing
In defibrillators older than the Lumax 740, a 50-ms analog blanking period begins after ventricular pacing during which no signal is sensed or visualised and a 215-ms digital blanking period during which the signal is not sensed though is visualised. Sensing begins at 2 mV for 85 ms after the end of blanking, then decreases to the programmed value of 0.8 mV. Starting with the Lumax 740 generation, a 19.5 ms analog blanking period begins after ventricular pacing and a digital blanking period of 120 ms. The upper threshold, which corresponds to a value equal to 50% of the post-pacing evoked response, is maintained for 400 ms. Then the sensitivity increases as the threshold falls to 25% (25% lower threshold) for 156 ms. The sensitivity then increases gradually throughout the cardiac cycle, with an additional -12.5% decrement every 156 ms, until the programmed sensitivity is reached.
Post pace T wave suppression
This option was introduced with the Lumax 540 model. A 2-mV sensitivity is maintained for a 300-ms period after ventricular pacing, while in the Lumax 740 model, the sensitivity is set by default at 3 mV and maintained for a 400-ms period after ventricular pacing. These settings can be changed by unlocking a code.
2- ProgrammING OF THE SENSING AND THERAPY ZONES
The setting of the defibrillator’s zones of heart rates that prompt the various therapeutic responses is a key programming step. State-of-the-art defibrillators enable the programming of several zones of arrhythmias detected on the basis of the sensed RR intervals. Each zone can be specifically programmed with respect to discrimination and therapies delivered. The number of zones and the range of heart rates that are programmed must be adapted to the characteristics, history and implant indications of each patient.
In the case of secondary prevention, in presence of heart failure, the programming of the heart rate zones is adapted to the cycle length of the VT that has prompted the device implant. The lower limit of the VT zone is usually programmed 20 bpm below the clinical VT, since the introduction of, or an increase in antiarrhythmic drug therapy after the implant may change the rate of the tachycardia.
In the case of primary prevention
In presence of heart failure, the risk of developing VT after device implant is considerable and probably justifies the programming of 2 zones of detection and treatment of tachycardia, besides a zone of VF. The main rationale for the programming of 2 separate zones of VT is the ability to treat very rapid tachycardias, specifically favouring painless antitachycardia pacing (ATP) over the delivery of electrical shocks, which represents a significant improvement in quality of life. These results justify the systematic programming of a sequence of ATP as initial therapy in the zone of fast VT.
In case of secondary prevention
In a patient in complete atrioventricular block
The risk of inappropriate therapy for a supraventricular tachycardia with conduction over the atrioventricular node is inexistent, allowing the setting of relatively slow heart rates prompting interventions by the device, without detriment to the specificity. The discrimination algorithms are unnecessary, as all spontaneous tachycardias are ventricular in origin.
In a young and active patient
The risk of inappropriate therapy for a normal acceleration of the heart rate, or for atrial fibrillation with rapid atrioventricular conduction must be taken in consideration when several treatment zones are being programmed, minimising overlaps of heart rates prompting defibrillator interventions and physiologic heart rates.
In a patient presenting with Brugada syndrom
Stable VT is extremely rare, whereas the risk of atrial fibrillation is increased. Consequently, the programming of a zone of detection and treatment of VT besides a VF zone is probably unnecessary and perhaps risky. The programming of an additional zone of monitoring only allows the recording of possible slower tachyarrhythmias and an adaptation of the setting. A single VF zone is usually programmed with a relatively rapid lower limit (> 210 bpm).
3-COUNT OF THE CYCLES AND DETECTION ZONES

The various ventricular events are classified as a function of the RR cycles during ventricular pacing, sinus rhythm, VT1, VT2 or VF. The lower limit of each zone is programmable, and the several zones are continuous. Each cycle in a tachycardia or VF zone increases the count by 1 in that zone, and the detection of a cycle in a fast zone increments by 1 the counter in a slower tachycardia zone. A cycle in the sinus zone decrements all prior counters by 1. When the counter has reached the number of required cycles (26 in the VT1 and 16 in the VT2 zone by default, 8 out 12 cycles in a sliding window in the VF zone), the diagnosis is made and the associated therapy is delivered.
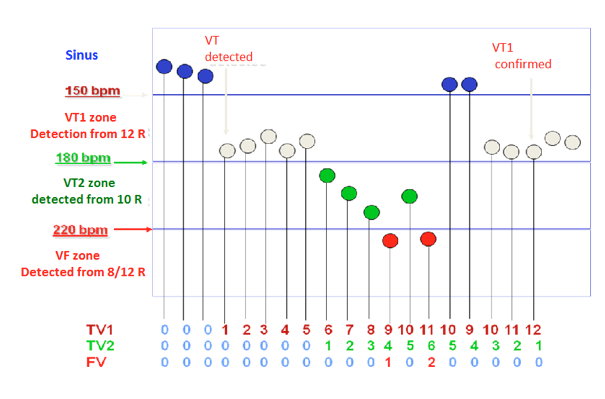
In this example, the counter of VT1 is filled first. A cycle in the sinus zone decrements by 1 the VT1 counter. A cycle in the VT2 or in the VF zone increments the VT1 counter by 1.
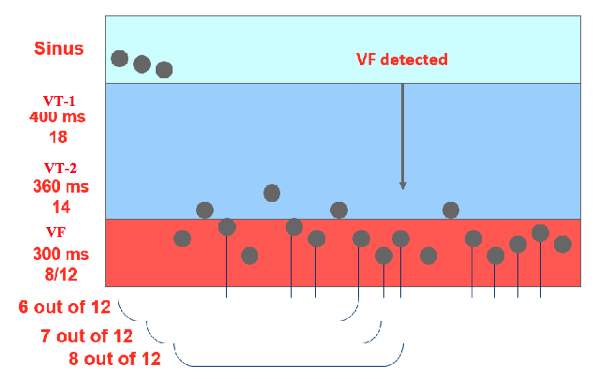
An episode of VF is detected when X out of Y (here 8 out of 12) intervals are shorter than the limit of the VF zone; 9 choices are programmable, from a shortest of 6 out of 8, to the longest of 24 out of 30 intervals.
4- RedEtection AND ED OF detection
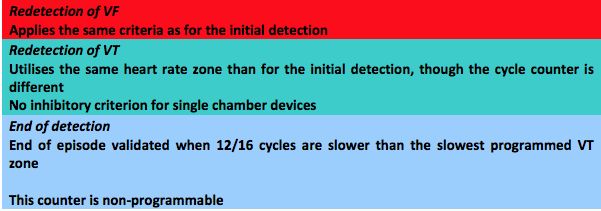
The phase of redetection begins when a therapy has been delivered. The programmed counts in the VT1 and VT2 zones must be lower than those applied in the initial detection in order to not delay the delivery of a new therapy when the first was unsuccessful (20 cycles for the VT1 and 14 cycles for the VT2 zone by default). The same X/Y cycles ratio is applied in the VF zone for the initial detection and the redetection.
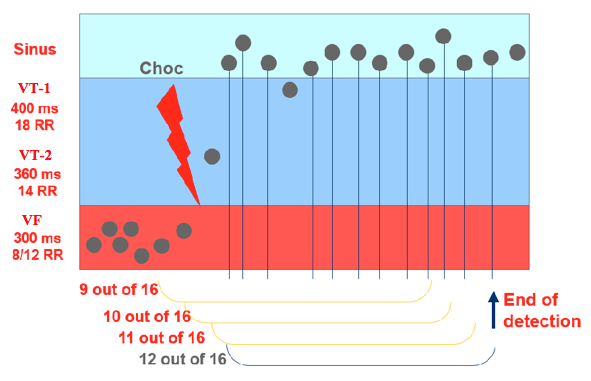
Example of redetection after delivery of a shock the VF zone; 12 of 16 cycles are in the sinus zone: end of episode.



