2:1 Block and Wenckebach behavior during exercise
Tracing
Manufacturer Medtronic
Device CRT
Field Effort
N° 13
Patient
Young patient (24 years old) implanted with a triple-chamber pacemaker Consulta CRT-P for a complete congenital AV block; dizziness during exercise; stress test performed on an ergometer with the telemetry wand placed over the device.

Graph and trace
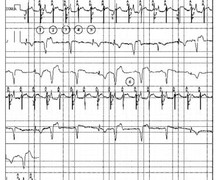
The first line corresponds to an electrocardiographic recording with superimposed markers, the second line to the bipolar RA EGM, the third line to the LV tip / RV ring (anode) EGM and the fourth line to a second electrocardiographic lead with the RR intervals; significant effort and dizziness with major dyspnea;
- atrial rhythm detected outside any refractory period (AS) and biventricular pacing;
- atrial rhythm detected falling in the PVARP (AR) and not followed by an AV delay or a biventricular pacing;
- alternating AS-BV-AR cycles; 2:1 block point is reached (one P wave on two falls in PVARP and is not followed); sudden drop in heart rate explaining the patients’ symptoms;
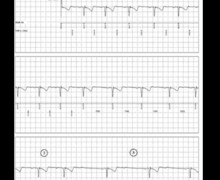
Programming change (rate adaptive AV delay and PRAPV auto) - P wave tracked with the prescribed AV delay (70 ms at peak exercise);
- progressive prolongation of the AV delay in order to maintain the HR at the maximum rate limit;
- marked prolongation of the AV delay; the BV-AS interval is relatively short although the atrial signal is not sensed in the PVARP; when programming a PRAPV in auto mode in young adults, it is important to select a short minimal PVARP (180 ms in this instance);
- the P wave falls in the post ventricular atrial blanking (Ab) and is therefore not followed by an AV delay or biventricular pacing; blocked P wave;
- Wenckebach behavior 8/7 (8 P waves for 7 BV pacings) with a progressive prolongation of the AV delay and 1 blocked P wave every 8 P waves;
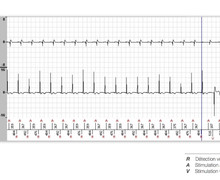
Programming change (maximum tracking rate is set at 180 bpm); - atrioventricular synchronization AS-BV 1/1.
Other articles that may be of interest to you




The specific settings in young CRT patients with a congenital atrioventricular block present certain peculiarities to be aware of. Indeed, in the vast majority of cases, retrograde conduction, as with anterograde conduction, is interrupted. This specificity must be integrated in the decision process regarding optimal programming, the risk of PMT being zero. A suitable adjustment must therefore enable preventing the occurrence of the 2:1 point during exercise, which is often associated with very disabling symptoms. In this patient, the 2:1 point was set too low. The total atrial refractory period, which defines the 2:1 point, corresponds to the sum of the AV delay + PVARP. In young patients, it is essential to push this 2:1 point beyond the capacities of sinus acceleration during exercise by programming a rate-adaptive AV delay with automatic shortening during exercise and the shortest possible PVARP, the majority of these patients not requiring protection from the risk of PMT, which can be considered nil. Setting a minimum AV delay to 70 ms and a PVARP to 180 ms allows pushing the 2:1 point well beyond 200 beats/minute.
The setting must also allow synchronization of biventricular pacing until the actual maximum tracking rate is reached by the patient. The Wenckebach behavior is most often less symptomatic than the 2:1 behavior although it must be avoided by setting a sufficiently high maximum tracking rate. In a CRT patient with a complete atrioventricular block and preserved chronotropic function, when the sinus rate accelerates and exceeds the programmed maximum tracking rate, ventricular pacing at the end of the programmed AV delay would be associated with an overshoot of the maximum tracking rate which is impossible. The ventricular rhythm can no longer follow the atrial rate in a 1:1 mode and plateaus around this value. To overcome this limitation, the device prolongs the AV delay and a Wenckebach operation of the device occurs. As the sinus frequency increases beyond the maximum tracking rate, the ventricular pacing rate remains at the maximum tracking value and the observed sensed AV delay is prolonged with each pacing cycle. When a sensed atrial event occurs during the PVARP, it is not synchronized with ventricular pacing, resulting in a missing beat. The following P wave falls outside of the refractory period and again initiates a programmed AV delay. This pattern is repeated for as long as the sinus rate remains above the programmed maximum tracking rate. Missing beats occur less frequently when the sinus rate is only slightly higher than the maximum tracking rate and more frequently when the sinus rate well exceeds the maximum tracking rate. Once the sinus rate falls below the maximum tracking rate, the 1:1 AV association is restored. The Wenckebach behavior can be defined by the rate at which the missing beat occurs and by the ratio of sensed atrial events over paced ventricular events (e.g., 8/7, 7/6, 6/5 or 3/2). Again, there is thus no reason to constrain the programmed maximum tracking rate below the patient's rhythm acceleration capacities during exercise.