Decrease in the percentage of biventricular pacing due to frequent premature ventricular contractions
Tracing
Manufacturer Medtronic
Device CRT
Field Management of atrial arrhythmias
N° 22
Patient
68-year-old man implanted with a triple-chamber defibrillator Viva XT CRT-D for ischemic cardiomyopathy with left bundle branch block; non-responder to cardiac resynchronization; percentage of biventricular pacing at 78%.
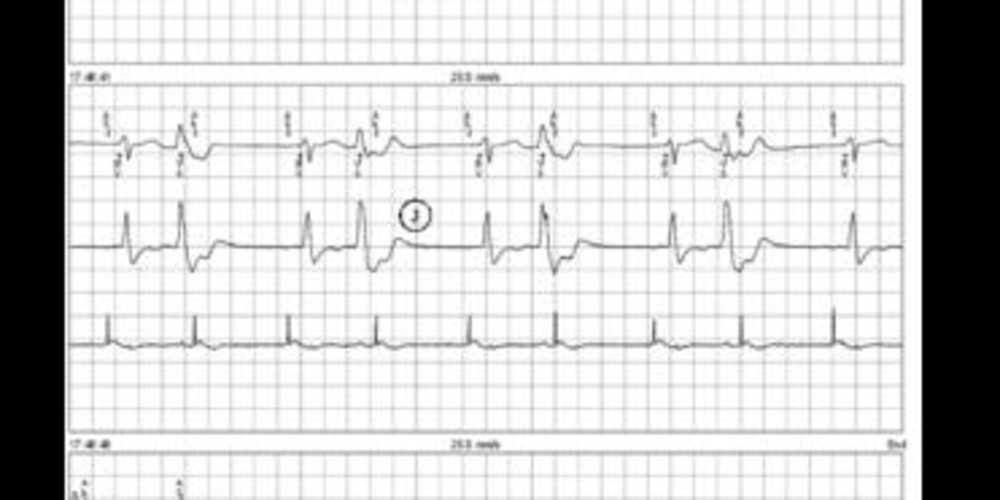
Graph and trace
The first line corresponds to an electrocardiographic lead with superimposed markers; the second line corresponds to the right ventricular EGM, and the third line to the right atrial EGM;
- sinus rhythm and biventricular pacing (AS-BV);
- PVC with atrial sensing included in the post ventricular atrial blanking;
- alternation between a biventricular pacing and a PVC: ventricular bigeminism susceptible to explain the decrease in the percentage of biventricular pacing;
- persistent ventricular bigeminism;
Programming change (increase in minimal heart rate from 55 to 70 bpm); - disappearance of the PVCs and percentage of ventricular pacing at 100% during the rest of the consultation.
Other articles that may be of interest to you

EGM recordings




Frequent premature ventricular contractions, isolated or paired, bigeminism or trigeminism, at rest or during exercise, is a common cause of the decrease in the percentage of biventricular pacing. It also causes a relative bradycardia as the PVCs are relatively ineffective from a hemodynamic standpoint. In a CRT patient, the evolution of the frequency of PVCs should be continuously monitored since they can be prompted by metabolic disorders and induced by drugs, or be the expression of a worsening underlying heart disease, or even at the origin of clinical decompensation. In non-responder patients, suppressing the PVCs is a priority so as to allow an increase in the percentage of biventricular pacing and thus anticipate a positive response to the resynchronization therapy. Different options are possible: