Delayed effect of a burst of ATP
Tracing
Manufacturer Abbott
Device ICD
Field Therapy
N° 35
Patient
This 60-year-old man presenting with ischemic cardiomyopathy, a 25% left ventricular ejection fraction and a wide QRS, received a Promote Accel triple chamber CRT-D for a primary prevention indication. He was seen for a routine ambulatory visit.
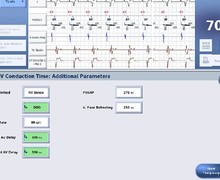
Main programmed parameters
- VF zone at 222 bpm, VT-2 zone at 190 bpm and VT-1 zone at 160 bpm
- 12 cycles in the VF zone, 12 cycles in the VT-2 zone and 12 cycles in the VT-1 zone were needed for the diagnosis
- Maximum sensitivity programmed at 0.3 mV
- VF zone: six 36-J shocks (maximum amplitude); VT-2 zone: 2 bursts followed by 1 ramp of ATP, followed by 3 shocks of maximal strength; VT-1 zone: 3 bursts followed by 3 ramps of ATP, followed by a single 15-J shock, followed by 2 shocks of maximal strength
- Effective discrimination in the VT-1 and VT-2 zones
- DDDR pacing mode at 55 bpm; DDI episode pacing mode; DDD post-shock pacing mode at 60 bpm

Graph and trace
Episode of tachycardia diagnosed in the VT-2 zone in the V>A arm and probably effective. Instead of being measured from the early post-therapy cycles, the post-therapy heart rate was measured from the 4 cycles preceding the diagnosis of return to sinus rhythm.
Tracing
- Atrial and biventricular pacing (AP-BP);
- Onset of irregular tachycardia with cycles initially unclassified or VS;
- DDI episode pacing mode after 3 T1 or T2 cycles;
- VT with cycle length alternating between VT-1 and VT-2 zones. Since the VT-2 counter (12 T2 cycles) was filled first, VT-2 was diagnosed. VT-2> means that the diagnosis was made in the V>A arm;
- Initial therapy in VT-2 zone: burst of 9 stimuli at a coupling interval equal to 85% of the tachycardia cycle length, calculated as the average of the last 4 cycles preceding the diagnosis;
- Continuation of the VT with slight acceleration of its rate;
- Delayed termination of the VT and diagnosis of return of sinus rhythm (after 3 VS).
Other articles that may be of interest to you
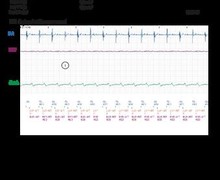





The success of ATP may be immediate or occur after a few cycles of tachycardia, as in this example. Either ATP was ineffective, and the VT ended spontaneously (in which case, in order to avoid ATP, the number of cycles needed for the diagnosis of VT should be increased, to increase the likelihood of spontaneous termination), or ATP has disorganized the VT, which caused its spontaneous termination. Despite the success of the therapy, one must, in this patient, be concerned about a possible proarrhythmic effect of ATP, and fear an acceleration of the tachycardia toward fast and sustained VT or toward VF.