Vagally-mediated syncope
A 48-year-old man presented with a several-year history of multiple syncopal events occurring in circumstances of enhanced vagal activity, such as after meals, or in church. The episodes were associated with prodromes, including perspiration and a sensation of warmth. He presented after 2 recent episodes of sudden loss of consciousness without prodrome, the latter complicated by a fall and facial trauma. The surface ECG revealed the presence of right bundle branch block and a tilt-table test elicited a mixed response, with bradycardia at 30 bpm and a precipitous fall in arterial pressure, followed by loss of consciousness. The prodromes were reminiscent of those associated with syncope occurring in the most distant past. Electrophysiological studies revealed the presence of a borderline HV interval at 68 ms. Because of the changes in the severity of symptoms and the borderline HV interval, a Reveal DX was implanted with remote monitoring.

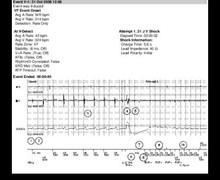
The remotely transmitted episode corresponded to the spontaneous symptoms reported by the patient. The recording was triggered by syncope preceded by postprandial prodromes. The graph provides an overall illustration of the episode, while the ECG recording allows a more precise diagnosis;
- the sinus rhythm is nearly regular at 60 bpm, with visible P-waves, albeit low in amplitude;
- noise was sensed, with a very short RR interval (FS), which, when repetitive, is ignored by the device (Ignored); the VR annotation indicates sensing during the ventricular refractory period; when several events are sensed consecutively in the refractory period, the interval is classified as a noisy interval; VS annotates an event that ends a noisy episode;
- rate acceleration to approximately 110 bpm; the mediocre quality of the recording with presence of noise and prominent variations in the ventricular electrograms are noteworthy;
- >3-sec asystole; the noisy baseline probably reflects the fall associated with syncope; while it is unclear whether the diagnosis is a sinus pause versus complete atrioventricular block, the former appears more likely; the double counting of ventricular electrograms is noteworthy;
- return to normal sinus rhythm;
- device activation by the patient (Symptom).
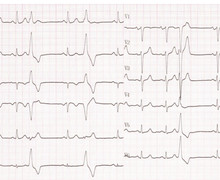




This and the previous recording show similarities. While the quality of this tracing is lower, hence complicating the distinction between atrioventricular block and sinus node dysfunction, the sinus rate accelerates before what appears to be a sinus pause considerably shorter than in the previous example. Thus, this tracing belongs to the IA classification of ISSUE. The clinical circumstances and the recording strongly suggest a vagally-mediated episode. However, whereas in the previous patient the length of the pause and frequent occurrence of the episodes appeared to support the implantation of a pacemaker, in this patient this recommendation was less clear. Some elements, in the present instance, were against the implantation of a pacemaker:
The point highlighted by this and the following cases is the importance of basing a decision to implant a pacemaker on the clinical context and individual characteristics of each patient, including when a pause is recorded at the time of a symptomatic event.