Unsuccessful ATP followed by electrical shock for VT
Tracing
Manufacturer Abbott
Device ICD
Field Therapy
N° 31
Patient
This 86-year-old man presenting with ischemic cardiomyopathy and 25% left ventricular ejection fraction, received a Current dual chamber ICD for secondary prevention (VT). He was seen in consultation for evaluation of palpitation followed by electrical shock.
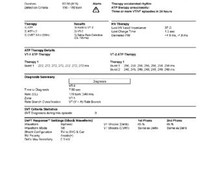
Main programmed parameters
- VF zone at 214 bpm, VT-2 zone at 171 bpm and VT-1 zone at 130 bpm
- 12 cycles in VF zone, 12 cycles in VT-2 zone and 20 cycles in VT-1 zone were needed for the diagnosis
- Maximum sensitivity programmed at 0.3 mV
- VF zone: six 36-J shocks (maximum amplitude); VT-2 zone: 3 ramps of ATP followed by single 5-J shock, followed by single 9-J shock, followed by 2 maximum shocks; VT-1 zone: 3 bursts of ATP followed by 3 ramps of ATP, followed by single 5-J shock, followed by 2 maximum strength shocks
- Effective discrimination in the VT-1 and VT-2 zones
- DDDR pacing at 65 bpm; DDI episode pacing; DDD post-shock pacing at 60 bpm

Graph and trace
Narrative
The narrative indicates that device diagnosed a VT-1 episode (V>A arm) lasting over 1 minute, with unsuccessful ATP sequences. Therapy sequences: 3 bursts of ATP at fixed heart rate and 10-ms decrement between each burst, followed by 3 ramps of ATP (with 10-ms decrement between each ramp), followed by 5-J shock (impedance = 48 Ohms). The shock was apparently successful and the heart rate slowed (cycle length = 855 ms).
Tracing
- The end of the previous episode is visible at the beginning of the EGM recording: unsuccessful burst with persistence of VT, though the heart rate (130 bpm) fell below the VT-1 zone, prompting an erroneous diagnosis of restoration of sinus rhythm (3 VS) and return to the programmed DDDR pacing mode;
- Subtle acceleration of the VT rate; DDI episode pacing mode after 3 T1, following restoration of sinus rhythm; the morphology is notably different from the reference morphology (x, 0);
- Diagnosis of VT-1 after 20 T1 cycles in the V>A arm;
- First burst of ATP;
- Unsuccessful burst, causing a slight slowing of the rate and VS or unclassified cycles, without diagnosis of restoration of sinus rhythm, however;
- VT-1 re-detection after 6 cycles (re-detection generally requires fewer cycles than the initial detection); second burst of ATP;
- Unsuccessful burst, slight prolongation of the VT cycle, with VS or unclassified cycles, though without diagnosis of restoration of sinus rhythm;
- Redetection and 3rd burst of ATP;
- Unsuccessful burst, redetection and 1st ramp;
- Unsuccessful ramp, redetection and 2nd ramp;
- Unsuccessful ramp, redetection and 3rd ramp;
- Unsuccessful ramp, redetection;
- Capacitors charge for 5 J (<1 sec charge time);
- In order for the shock to be delivered, ≥6 fast T or F cycles must be confirmed, explaining the delay at the end of charge before delivery of the 5-J shock;
- Successful shock and diagnosis of restoration of sinus rhythm.
Other articles that may be of interest to you
EGM recordings





In this patient, the following sequence of therapies was programmed in the VT-1 zone:
3 sequences of bursts of ATP, followed by 3 sequences of ramps of ATP, followed by a single 5-J shock, followed by 2 maximum energy shocks. These therapies followed each other in case of consecutive failures. The sequence ends as soon as the rhythm is considered slow again, or when all therapies have been exhausted.
The choice of amplitude of the first shock might be discussed: it can be empirically programmed at a low amplitude with a view to terminate the tachycardia while limiting the pain caused by the electrical shock and minimising the energy consumption. The shock strength must not be programmed below 5 V in order to not fall below the atrial or ventricular upper limit of vulnerability, and risk of precipitating AF or VF. An alternate choice consists of programming a first shock of maximum strength, with a view to increase the likelihood of VT termination at first attempt, decreasing thereby the number of shocks delivered to a maximum and increasing the probability of terminating AF, should the shock be inappropriate.