post-ventricular atrial blanking and crosstalk
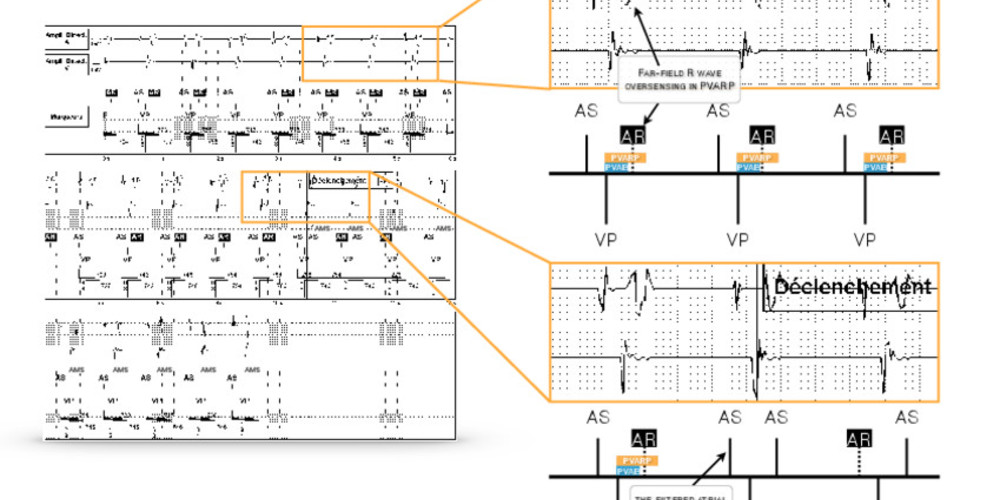
74-year-old woman, implanted with an Assurity MRTM dual-chamber pacemaker for complete atrioventricular block; during the interrogation, highlighting of an episode of automatic mode switching (AMS) stored in the device memory.

At the beginning of the tracing, atrial sensing (AS) and ventricular pacing (VP); after each ventricular pacing, presence of a signal sensed by the atrial channel with a fixed coupling; probable crosstalk; the oversensed signal falls in the PVARP (AR) and therefore does not trigger an AV delay but is counted for the assessment of the filtered atrial rate; this succession of cycles with crosstalk leads to mode switching (AMS) in DDIR mode; loss of atrioventricular synchrony (DDIR mode, no ventricular synchrony on sensed P wave).
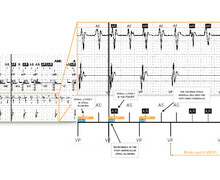




Following ventricular pacing, atrial sensing is inhibited for the duration of the post-ventricular atrial blanking period in order to avoid crosstalk. This blanking must be programmed sufficiently long to avoid sensing of the stimulus but also to avoid sensing of ventricular depolarization by the atrial channel. It should not be programmed too long in order to avoid undersensing of a possible episode of atrial arrhythmia as on the previous tracing. Following this blanking, the PVARP begins, where a signal is sensed and is counted for the atrial arrhythmia diagnosis but does not trigger an AV delay to avoid the risk of PMT.
In this patient, ventricular depolarization is systematically oversensed (in the PVARP) by the atrial channel. Repetition of these cycles leads to mode switching. The Fallback function on AbbottTM devices is based on an analysis of the filtered atrial rate interval. A short cycle decrements this interval by 38 ms while a long cycle increments the interval by 25 ms. The succession of atrial cycles presented by this patient (short cycle, long cycle) results in a systematic 13 ms incrementation of the filtered atrial rate interval. The latter progressively reaches the threshold for mode switching which results in the loss of atrioventricular synchrony.
In this patient, it is possible to prolong post-ventricular atrial blanking so as to prevent this signal from being counted in the computation of the filtered atrial rate interval or to reduce atrial sensitivity. These 2 options can be accompanied by an altered sensing of AF (primarily for the reduction in atrial sensitivity) or 2:1 atrial flutter (primarily for prolonging atrial blanking).