Heart rate drop during exercise
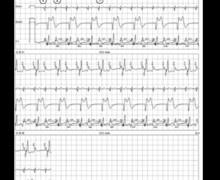
Tracing
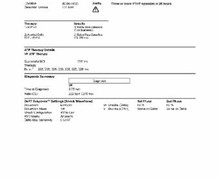
Manufacturer Biotronik
Device PM
Field Programming for exercise
N° 27
Patient
53-year-old man implanted with an Evia DR-T dual-chamber pacemaker for complete atrioventricular block; feeling of lipothymia on exertion; performance of an exercise test at consultation (repeated flexions).

Graph and trace
Tracing 27a
- onset of exertion; atrial sensing and ventricular pacing; analysis of the pattern of the atrial electrograms reveals a variable amplitude, even if all P waves are sensed;
- discomfort experienced by the patient; atrial undersensing (P wave not sensed); low amplitude signal; in the absence of atrial sensing, no ventricular pacing and pause (ventricular rate divided by 2) explaining the discomfort felt by the patient;
- respiratory cycle of the atrial signal amplitude; P waves properly sensed;
- new atrial undersensing due to a low-amplitude signal and sudden decrease in ventricular rate;
- continuation of exertion; marked lipothymia; improvement in the quality of atrial sensing (signals of greater amplitude); atrial sensing and ventricular pacing;
- P wave sensed in the PVARP; absence of ventricular pacing;
- 2:1 point; repetitive sequences with every second P wave falling within the PVARP;
- change in programming: shortening of the PVARP;
- resumption of atrioventricular 1:1 synchrony and of a physiological and adjusted rate; disappearance of symptoms;
Tracing 27b
Atrial sensing test (VDI 30 bpm)
- this test shows the variability in the measurement of the atrial signal amplitude (between 1 and 2.7 mV).
Other articles that may be of interest to you
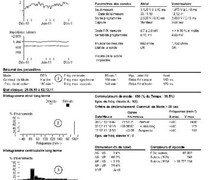


This patient presented significant symptomatology on exertion with the presence of lipothymias and marked limitation of his exercise capacity. Several mechanisms can be involved in this setting. The particular interest of this tracing is that the exercise revealed both an atrial undersensing and a 2:1 block.
This patient presented an intermittent atrial undersensing. Atrial EGM analysis revealed a wide variability in the amplitude of atrial signals as a function of the respiratory rhythm. In a patient with preserved atrioventricular conduction, an atrial undersensing on exertion is associated with a reappearance of spontaneous ventricular activity without a sudden fall in rate and therefore without significant symptomatology. Conversely, in a patient with complete atrioventricular block (as on this tracing), atrial undersensing results in a sudden drop in rate, which is often symptomatic. Atrial undersensing is much more frequent than a 2:1 block or ventricular oversensing or loss of capture of the 2 leads, which constitute the other causes of a sudden drop in rate on exertion and should therefore be searched in priority in this setting. For a recent BiotronikTM dual-chamber pacemaker, atrial sensitivity can be programmed to a fixed value or with automatic adjustment (automatic sensitivity control). The automatic sensitivity control measures the amplitude of the P wave and adjusts the cycle to the sensitivity threshold. The maximum automatic sensitivity is 0.2 mV for atrial bipolar sensing and 0.5 mV for atrial unipolar sensing (non-modifiable). In this patient, atrial sensing was programmed to a fixed value of 0.5 mV. A programming change to an adaptive sensitivity corrected the problem.
This tracing also allows emphasizing the specifics of the settings in patients with preserved exercise capacity and complete atrioventricular block. An adjusted setting should avoid the occurrence of the 2:1 point, which often leads to disabling symptoms. In this patient, the 2:1 point was set too low (150 bpm). The total atrial refractory period that defines the 2:1 point corresponds to the sum of the AV delay + PVARP. In young patients, it is essential to push this 2:1 point beyond the sinus acceleration capacities during exercise. To achieve this, it is possible to program a dynamic AV delay with automatic shortening upon exertion. In this complete anterograde atrioventricular patient, a 90-bpm VDD test did not demonstrate retrograde conduction during 3 successive consultations making the occurrence of a PMT highly hypothetical (possible but very unlikely resumption of a prior retrograde conduction essential for the occurrence of a PMT). It therefore appears possible to program an extremely short PVARP, which allows to considerably increase the 2:1 point and thus restore a preserved exercise capacity.