Medtronic Therapies
In this article
Implantable defibrillators have been historically developed to prevent the risk of sudden death and reduce malignant ventricular arrhythmia by electrical shock. In the VF zone, a maximum of 6 shocks can be delivered for a single episode. While the amplitude of each of the shocks can be programmed independently, it is customary to program an amplitude at maximum capacity of the device (35 Joules) for shocks 2 to 6. In contrast, the amplitude of the first shock can either be programmed to the maximum capacity of the device, or to a value lowered by 10 Joules (25 Joules), or to a lower amplitude tested during an induction procedure. Programming a first shock of average amplitude (between 15 and 20 Joules) allows shortening the charging time and the delay between the onset of the arrhythmia and the delivery of the electrical shock and, in certain specific cases, can reduce the risk of loss of consciousness (an important problem for drivers, for example). The choice of the amplitude of the first shock in the VF zone therefore represents a compromise: an average energy may suffice to terminate the VF after a short charging time, however if unsuccessful, the second maximum energy shock will be delivered after a long total VF time; an immediate high energy will be more efficient on the VF, but at the cost of a longer initial charging time.
At the end of charging for the first shock, there is a confirmation phase after which the shock is delivered. Following this shock, a blanking phase of 520 ms is initiated with no possible sensing and a 1200 ms phase with no possible pacing in order to avoid the risk of pacing during a vulnerable period if a QRS complex is not sensed during the blanking.
Committed shock
If the shock is unsuccessful and the device redetects a VF episode, the second charge begins and the shock is irrespectively delivered (“committed shock”) at the end of the charge even if termination was achieved in a second instance as demonstrated in this example. Indeed, the probability of a spontaneous termination is low after a first unsuccessful shock, the device suspecting a possible prolonged ventricular undersensing responsible for an erroneous diagnosis of a return to sinus rhythm. At the end of this second charge, a 900 ms window begins. If a ventricular complex is detected in this window, as in this example, the shock is delivered synchronously; if no ventricular complex is detected, the shock is delivered asynchronously at the end of this window.
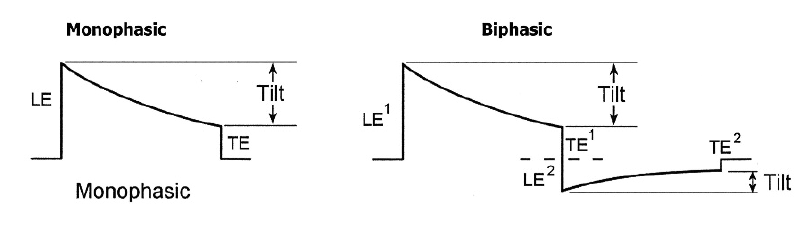
Shock waveform:
The shock waveform is not programmable on MedtronicTM devices, the electrical shocks delivered are necessarily biphasic without possible modification; indeed, while the first available devices delivered monophasic shocks, the introduction of biphasic shocks on the more modern platforms have enabled to significantly reduce the defibrillation thresholds and the risk of re-induction. The direction of the shock waveform is reversed with a non-modifiable 50/50 tilt. The polarity can be programmed independently for the 6 shocks of the series with 2 possible options: B>AX and AX>B; B corresponds to the right ventricular coil and AX to the active can and superior vena cava coil; in anodic shock (B>AX), the right ventricular coil constitutes the anode for the first phase and the cathode for the second; conversely, in cathodic shock (AX>B), the right ventricular coil constitutes the cathode for the first phase and the anode for the second phase.
Shock vector:
Most state-of-the-art ICDs allow the programming of shock polarity. This may be useful to lower a high defibrillation threshold. Programming of the shock polarity depends on the number of high voltage electrodes available. The defibrillation shock is delivered via a dedicated lead, which may have a single coil positioned in the right ventricle, or a dual coil with a distal component placed in the right ventricle and a more proximal component in the superior vena cava. With a single coil lead, the shock is delivered between the distal anodal coil in the right ventricle and the cathodal can of the pulse generator. A dual coil lead allows delivery of shocks between the distal coil, the proximal coil and the can. The nominal setting uses the 2 transvenous coils as anode and the can of the pulse generator as cathode. The shock vector can be changed by changing the polarity of the electrodes. For example the coils can be programmed as the cathode and the can as the anode. Or the can is disabled and the energy is delivered between the 2 coils of the defibrillation lead, or the proximal coil is disabled and the shock is delivered between the distal end or the lead and the can. Shock polarity may be also be reversed between each shock.
Shock energy:
In the VF zone, the first and subsequent shocks are usually programmed to the maximum output of the device. Programming of the shock energy can be guided by the defibrillation threshold, defined as the lowest energy required to defibrillate the heart. In the VT zones, the first shock can be programmed empirically to 5 to 10 J, which saves the battery and shortens the charge of the capacitor, or to higher energies to increase the likelihood of VT termination.
Formatting the capacitors:
The capacitors are regularly formatted to keep the charge time short, since it increases in the absence of charges. However, in order to spare the battery, the automatic formatting process is postponed each time a full charge has occurred. When the charge time exceeds 16 seconds, the device reforms the capacitors every month. If a second charge time exceeds 16 seconds, the device displays an ERI warning.
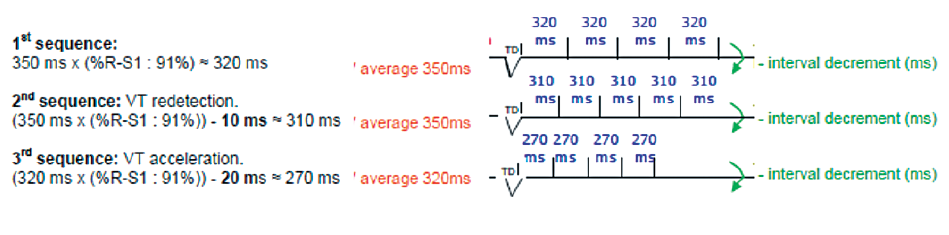
Medtronic proposes 3 types of sequences: burst, rampe or rampe+.
BurstIn a burst the number of impulses is similar for every sequence, although one impulse can be added to every sequence, yet the interval time duration remains constant between two impulses within a sequence.
Burst : example
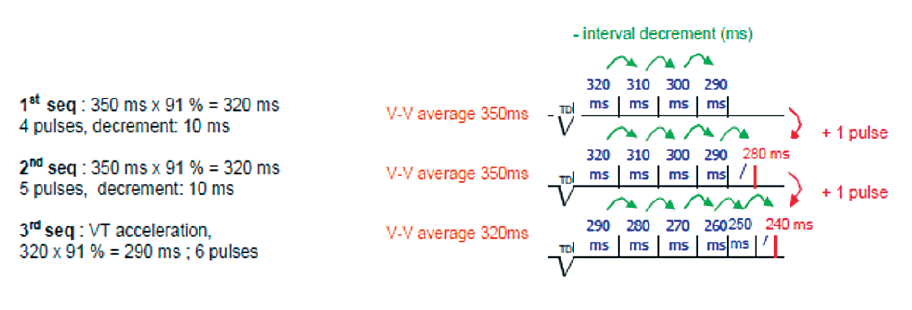
In a ramp, one impulse is added to every sequence, the interval time duration reduces by the programmed decrement value from one impulse to another.
Atrial activity sensing allows for continuous and stimultaneous comparison of the atrial rate and the ventricular rate.
Ramp : example
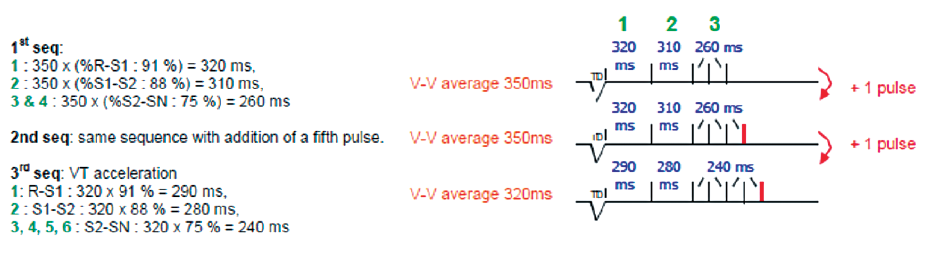
In a ramp+, a pulse is added to each sequence, reducing the length of intervals for the first 3 pulses and then remaining constant thereafter.
Ramp+: example
Traditionally, a VF zone was programmed for high heart rates (lower limit at 188-200 beats/minute) with a high amplitude electrical shock as first therapy. Various studies have shown, however, that a significant proportion of fast ventricular arrhythmias (cycle duration <320 ms) and classified in the VF zone are regular and monomorphic (fast VT potentially treatable by anti-tachycardia pacing). While the efficacy of an electrical shock in terminating rapid ventricular arrhythmia is unarguable, it is nonetheless painful and significantly increases energy consumption. The delivery of several successive shocks in a same patient is thus associated with a risk of premature depletion of the batteries and a significant lowering of the quality of life of the patients (many described cases of depression or anxiety induced by a series of shocks) as well as an altered prognosis (mortality risk increases in parallel with the number of shocks delivered).
The PainFREE Rx trial (prospective, randomized, multicenter study) showed that a single anti-tachycardia pacing sequence (8 beats at 88%) allowed terminating a large proportion of fast tachycardias in the VF zone and provided a significant benefit in terms of quality of life, by reducing the number of shocks delivered without increasing the risk of sudden death, syncope or accelerated tachycardia. Thus, delivering an anti-tachycardia pacing sequence in the VF zone often appears to be effective, painless, prolongs battery longevity and improves the quality of life, and should therefore be offered as a first-line option for this range of tachycardias (< 250 beats/minute). It is now recommended to program at least one anti-tachycardia pacing sequence as first treatment for tachycardias up to a rate of 230 beats per minute by favoring burst rather than ramp therapy (at least 8 stimuli with 88% coupling).
ATP during charging
ATP during charging enables painless treatment of ventricular tachycardia without the risk of delaying shock treatment when necessary. Once the diagnosis of VF is established, the charge begins and ATP is delivered simultaneously. If thereafter, VF is reconfirmed, the shock is delivered. If the patient has returned to sinus rhythm, the shock is withheld. This hence allows treating tachycardia painlessly if the ATP is successful, without delaying the onset of shock if the ATP is unsuccessful. However, even if it is successful, ATP saves little energy. ATP before charging reduces energy consumption. Once the diagnosis of VF is established, ATP is delivered. If VF is reconfirmed after ATP, the capacitor begins charging. If the arrhythmia has been terminated, the charge is not initiated. This allows withholding charging of the capacitors if the ATP is successful. On the other hand, if ATP is unsuccessful, it delays shock delivery by a few seconds. The device delivers the ATP before or during the charge only if the last 8 detected ventricular intervals are equal to or longer than the programmed value (“Deliver the ATP if last 8 RR ≥”). If one programs the charge saver, the device automatically switches from an ATP delivered during charging to an ATP before charging if the former has been successful on a programmable number of consecutive episodes.
A priority in the programming of an implantable defibrillator is to minimize the delivery of shocks as much as possible without compromising patient safety. Ideally, this entails terminating the tachycardia with the least aggressive and least painful treatment modality possible. Anti-tachycardia pacing is therefore favored as first-line therapy for organized tachycardias comparatively to electrical shocks, being less painful and lowers battery consumption and wear. Moreover, the deleterious effect of electrical shocks has been clearly demonstrated. The principle behind anti-tachycardia pacing is to capture the arrhythmia and interrupt an organized VT by penetrating its propagation circuit through the ventricles. The ventricle must hence be paced at a faster rate than that of the tachycardia. The efficacy of this type of therapy has been demonstrated for a wide range of VT rates up to 240 beats/minute and has consistently been shown to terminate nearly 90% of slow ventricular tachycardias with a rate of less than 200 beats/minute and a moderate risk (1 to 5%) of acceleration. These observations have repositioned the ICD as a first-line treatment of arrhythmias by rapid pacing with the possibility of defibrillation as “back-up” only as needed.
Various parameters must be programmed: 1) the type of sequence: in a burst, the duration of the intervals is constant during a sequence (no change in rate from one stimulus to another). This is the type of sequence most commonly used in clinical practice and probably the least aggressive. According to the new guidelines, the burst should be preferred to other types of sequences. In ramp therapy, the interval is reduced from one stimulus to the other by the decrement value which is programmable. In ramp+ mode (specificity of this manufacturer), a pulse is added to each sequence, reducing the length of the intervals for the first 3 intervals and remaining constant thereafter; 2) the number of programmed sequences varies according to the rate of the tachycardia. In a slow VT zone (<150 beats/ minute), it is possible to program a large number of sequences so as to delay the delivery of a shock to a tachycardia that does not generally threaten short-term survival. It is also possible to not program an electrical shock in this slow VT zone. For tachycardias between 150 and 200 beats per minute, it is common to program 3 to 6 successive sequences of anti-tachycardia pacing; 3) the number of pulses per sequence: on average, 5 to 15 consecutive pulses are programmed for each burst. If the number is insufficient, the pacing sequence may not penetrate the tachycardia circuit and the burst is unsuccessful. On the other hand, if the number is too high, the risk is terminating and subsequently re-inducing the tachycardia. An additional stimulus can be systematically added from one sequence to another. According to the new recommendations, a minimum of 8 stimuli per sequence should be programmed; 4) the value of the coupling and pacing intervals: the shorter the coupling intervals, the more aggressive the therapy and the greater the risk of accelerating the tachycardia. According to the new recommendations, for a burst, an 88% coupling relative to the rate of the tachycardia (calculated over the last 4 cycles before diagnosis) must be programmed; 5) the minimum coupling allows limiting the aggressiveness of a pacing sequence; there is a programmable rate limit above which, irrespective of the programming, the device does not deliver pacing. When, for example, during a ramp, the minimum coupling is reached, the subsequent intervals are paced with this minimum coupling without additional decrement; 6) the pacing amplitude and the pulse duration can be programmed independently so as to promote effective capture during the tachycardia; 7) the pacing site(s) can be programmed; the pacing site is necessarily right ventricular in a single or dual-chamber ICD. In a triple-chamber ICD, pacing can be delivered in the RV, LV or biventricular. From a theoretical perspective, biventricular or left ventricular pacing appears to be superior in patients with left ventricular dysfunction, with the majority of tachycardias originating in the left ventricle (less distance between the reentrant/tachycardia circuit and the pacing site); 8) it is also possible to program the Smart Mode to turn off a therapy when it has proven ineffective. This algorithm deactivates an anti-tachycardia pacing sequence that has been unsuccessful for 4 consecutive episodes (varies according to platform). An additional option is the programming of the progressive therapy algorithm which ensures that each therapy delivered for a single episode is at least as aggressive as the previous therapy.


