Ventricular sensing failure
Tracing
Manufacturer Biotronik
Device PM
Field Sensing
N° 22
Patient
84-year-old man implanted with a Biotronik Cyclos DR pacemaker for atrial disease; asymptomatic, routine visit.

Graph and trace
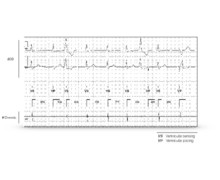
Tracing 22a
- atrial sensing and ventricular pacing with possible fusion with spontaneous rhythm;
- unsensed PVC (no marker);
- atrial sensing and ventricular pacing in the post-PVC T wave (vulnerable period) without effective capture;
- atrial sensing and ventricular pacing with possible fusion with spontaneous rhythm;
- unsensed PVC (no marker);
- atrial sensing and ventricular pacing in the post-PVC T wave (vulnerable period) with effective ventricular capture and arrhythmogenic risk;
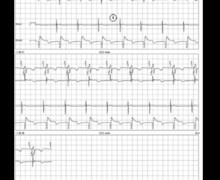
Tracing 22b
Ventricular sensing test (VVI 40 bpm);
- proper ventricular sensing of the conducted ventricular activity (pattern confirming the preceding fusion pattern);
- sensed PVC;
- unsensed PVC;
Tracing 22c
Programming change in ventricular sensitivity (pacemaker rendered more sensitive, lowering of the programmed sensitivity value);
- proper sensing of PVC.
Other articles that may be of interest to you





Device sensitivity expressed in millivolts (mV) qualifies the ability of the pacemaker to correctly sense spontaneous cardiac events. An adequate programming of the sensitivity level should detect all spontaneous cardiac events occurring in the implanted chamber while not detecting other events (crosstalk with sensing of cardiac signals from the other chamber, myopotentials, interference, etc). The programming of bipolar sensing allows increasing the specificity of the sensing relative to unipolar sensing by limiting the risk of sensing extracardiac signals or crosstalk while enabling the programming of high sensitivity values. Conversely, in the unipolar configuration, the risk of sensing extracardiac signals or crosstalk requires the programming of a lower sensitivity level with an increased risk of undersensing.
Traditionally, unlike implantable defibrillators, pacemakers operated with a stable and fixed sensitivity over the entire cardiac cycle. Nowadays, the various manufacturers offer in their range of devices a fusion between the operating platforms of both pacemakers and defibrillators. Although the sensing constraints differ (crucial need for a defibrillator to detect and treat very rapid, polymorphic and low-amplitude ventricular rhythm disorders), modern pacemakers allow the programming of an adaptive sensitivity (variable sensitivity level according to the amplitude of the sensed R wave or P wave) with a progressive increase in sensitivity during the cardiac cycle (possibility of detecting small amplitude signals without oversensing the T wave).
For BiotronikTM pacemakers, atrial and ventricular sensitivity can be programmed to either a fixed value or with automatic adjustment (automatic sensitivity control). The maximum automatic sensitivity is 2 mV for the ventricle (higher value than for a defibrillator), 0.2 mV for atrial bipolar sensing and 0.5 mV for atrial unipolar sensing. Following a pacing pulse, the maximum sensitivity is achieved after 360 ms in the atrium and 575 ms in the ventricle. When ventricular sensitivity is programmed to automatic, the maximum sensitivity value is therefore not programmable (2 mV non-modifiable value).
These tracings reveal an undersensing of PVC leading to pacing in the vulnerable period. The depolarization signal of an extrasystole is often fragmented, the slopes of its various components often being slower, with an increased risk of undersensing. In the absence of proper sensing, the pacemaker operates in asynchronous mode with no possible inhibition on spontaneous ventricular activities. There is a small but non-zero theoretical risk of inducing a malignant polymorphic ventricular arrhythmia compromising patient survival. In addition, this unnecessary and dangerous pacing leads to energy consumption detrimental to the lifespan of the device. Programming a more suitable fixed ventricular sensitivity allowed correcting the problem. The choice between automatic sensitivity and fixed sensitivity is sometimes difficult. Programming a fixed ventricular sensitivity of 1 or 2 mV renders the device more sensitive than programming to automatic sensitivity. In the presence of an oversensing or undersensing problem, the choice of the sensing method (fixed or adaptive) will primarily depend on the amplitude of the signals and the variability in amplitude of these signals.