Blanking, safety window, AV delay
Tracing
Manufacturer Medtronic
Device PM
Field AV delays, refractory periods management of tachycardia
N° 4
Patient
This 61-year-old man received a dual chamber pacemaker programmed in DDD mode for management of syncope due to paroxysmal sino-atrial block; he was seen for routine follow-up and the following tracings were recorded.
Graph and trace
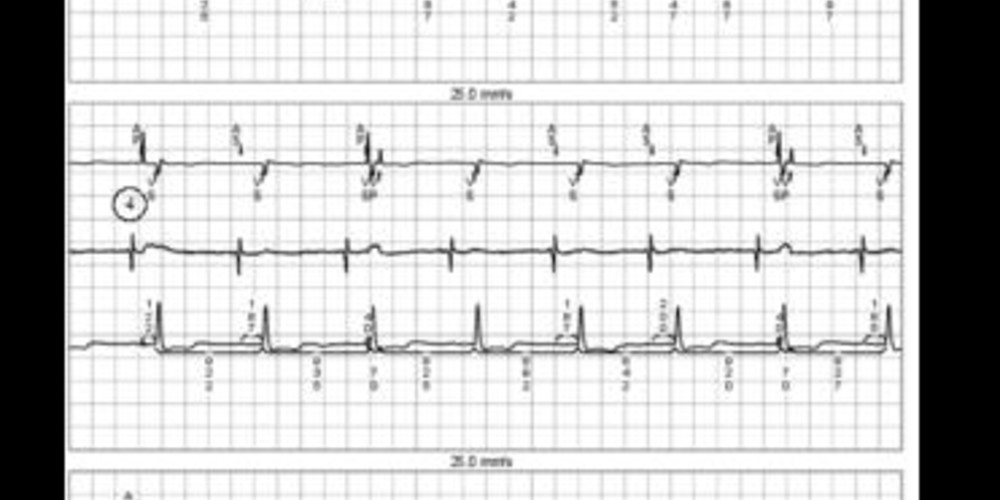
The first channel is lead III of the surface ECG upon which the markers are superimposed, the second shows the atrial EGM, and the third is lead II with the markings of the time intervals;
- 1: accurately sensed AS-VS cycle;
- 2: atrial undersensing; the atrial EGM channel shows that the atrial signal is not sensed by the pacemaker; in absence of atrial sensing, the atrium is paced (AP) at the end of the escape cycle; the spontaneous QRS originating from the non-sensed atrial event falls just behind AP, in the post-atrial pacing ventricular blanking period; therefore, this spontaneous ventricular event is not detected and does not trigger ventricular pacing at the end of the safety window; ventricular pacing is, therefore, triggered at the end of the AV delay, though is ineffective; this paced event is risky, as it falls on the T wave of the preceding spontaneous QRS complex;
- 3: same sequence: atrial undersensing, atrial pacing and spontaneous ventricular event; this time, the spontaneous ventricular event does not fall in the blanking period rather than in the safety window; consequently, it is sensed and triggers a paced event at the end of the safety window, which is ineffective and innocuous, as it falls during the absolute refractory period of the preceding spontaneous ventricular complex;
- 4: same sequence: atrial undersensing, atrial pacing and spontaneous ventricular event; the latter is neither in the blanking period nor in the safety window, but at the end of the AV delay and, therefore, inhibits ventricular pacing;
- 1: atrial pacing (AP) at the backup rate at the end of the 1,000 ms escape cycle between 2 atrial paced events;
- 2: accurate sensing of an atrial extrasystole (AS) and resetting of the atrial escape cycle; 3: accurately sensed blocked atrial extrasystole, though not followed by ventricular pacing; resetting of the atrial escape cycle ending with an atrial paced event in absence of other sensed atrial event
Other articles that may be of interest to you
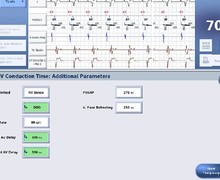





This tracing illustrates the occurrence of intermittent atrial undersensing in absence of other functional abnormalities. It shows the 3 ventricular intervals that follow atrial pacing, i.e. the blanking period, the safety window and the end of the AV delay; it shows the pacemaker’s response to a ventricular event falling during one of each of these intervals. The duration of the safety window is not programmable and is fixed at 110 ms. On the other hand, the duration of the blanking period can be changed. If programmed too short, the risk of detection of the atrial stimulus in the safety window is high, constantly forcing a ventricular paced event with an AV delay of 110 ms. This excessively short AV delay can be hemodynamically deleterious. If the blanking period is programmed too long, a late ventricular extrasystole might not be sensed, creating a high risk of pacing in its vulnerable period, at the end of the AV delay (a ventricular extrasystole falling during the blanking period does not modify the behaviour of the pacemaker, which paces at the end of the programmed AV delay). This risk increases with the programming of long blanking periods and long AV delays. An acceptable compromise is usually reached by programming a blanking period between 30 and 40 ms. In this patient, the actual problem is that of intermittent atrial undersensing, which was solved by a resetting of the atrial sensitivity.