Automatic atrial threshold measurement
Tracing
Manufacturer Biotronik
Device PM
Field Pacing
N° 21
Patient
77-year-old man implanted with an Evia DR-T dual-chamber pacemaker for syncope with left bundle branch block; during the consultation, automatic right atrial threshold measurement.
Graph and trace
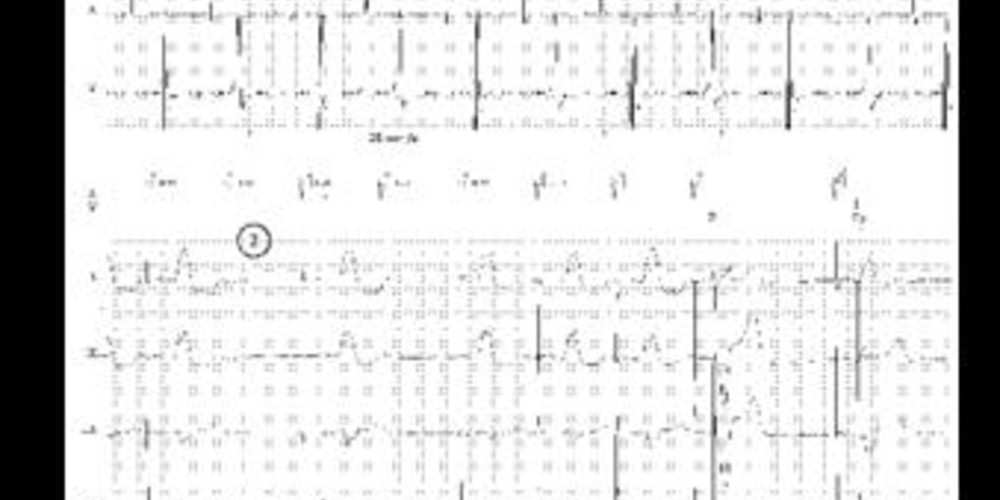
Tracing 21a: manual measurement of the right atrial threshold
- pacing in the AAI mode with capture verification by the presence of ventricular conduction; 0.1 V step over 2 cycles; effective capture;
- loss of capture at 0.3 V (threshold measured at 0.4 V);
Tracing 21b: automatic measurement of the right atrial threshold
- the threshold measurement is carried out in DDI mode (no ventricular trigger of spontaneous atrial activities and therefore no risk of PMT) at a rate 20% higher than the spontaneous rate (in order to favor atrial pacing) with a short AV delay of 50 ms and a post-ventricular atrial blanking of 150 ms (compromise in order to avoid crosstalk and to favor atrial sensing indicating loss of atrial capture); for each tested value, 5 pulses are delivered; the starting value is programmable (in this instance 3 V, nominal value); in the absence of atrial sensing, diagnosis of effective atrial capture;
- reduction of pacing amplitude in decremental 0.6 V steps (in each instance, 5 pulse tests);
- for an amplitude of 0.6 V, persistence of the capture (absence of sensing of spontaneous atrial activity);
- prior to decreasing the amplitude, atrial synchronous pacing delivered at the end of each series of 5 pulses; this atrial pacing is of an amplitude greater than 0.5 V relative to the previous tested amplitude;
- reduction of amplitude in decremental 0.1 V steps with capture at 0.3 V;
- new atrial synchronous pacing;
- loss of capture diagnosed upon the presence of spontaneous atrial activity (traced line on the atrial markers line);
- after 2 consecutive losses of capture, synchronous pacing;
- to verify this threshold measurement: first step, 5 pulses at an amplitude above 0.3 V relative to the threshold value; in this instance, 0.7 V since threshold measured at 0.4 V (last effective value); with this margin, capture is effective;
- second step, 5 pulses at an amplitude under 0.3 V relative to the threshold value; in this instance, 0.1 V since threshold measured at 0.4 V (last effective value); with this margin, the absence of capture is verified;
Other articles that may be of interest to you
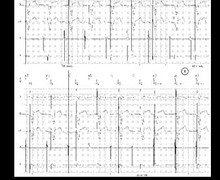






In this patient, the measurement of the automatic atrial threshold reveals the same value as that performed by the physician, thus validating the proper functioning of the automatic threshold measurement algorithm. The functioning of the automatic atrial threshold measurement and the ensuing amplitude adjustment have many similarities with the control of ventricular capture but also certain differences. The automatic control of atrial capture is not based on the analysis of the evoked atrial response but on the presence of sensed atrial signals indicative of loss of capture: resumption of intrinsic rhythm or retrograde conduction if the patient is dependent on the atrium (sinus dysfunction). This measurement cannot therefore be performed in patients with major sinus dysfunction and with no retrograde conduction. The combination of a short AV delay and a short post-ventricular atrial blanking allows optimizing the atrial sensing window while reducing the risk of crosstalk which can distort the measurement. The atrial threshold test procedure generally lasts longer (for an equal threshold value) than the ventricular threshold measurement.
The programmable parameters remain the same (possibilities of ON, OFF and ATM) although certain nominal values differ: minimum amplitude (nominal value of 1 V), safety margin (nominal value of 1 V).
The principle of amplitude adjustment once the threshold is measured is fundamentally different since it is based on the Auto-threshold concept. The atrial threshold is measured one or several times a day (time of measurement and number of measurements per day are programmable). There is then no cycle-to-cycle verification of capture efficiency although the amplitude is adjusted until the next measurement (fixed amplitude between 2 threshold measurements). This explains why the programmed safety margin is greater (adjustment to circadian threshold variations) than the automatic ventricular adjustment.