VDD and DDD modes
Tracing
Manufacturer Abbott
Device PM
Field Pacing Modes
N° 1
Patient
75-year-old man implanted with an AssurityTM + DR pacemaker for episodes of syncope due to paroxysmal atrioventricular block; well positioned leads with proper pacing and sensing thresholds; programming of various pacing modes and recording of the tracings.
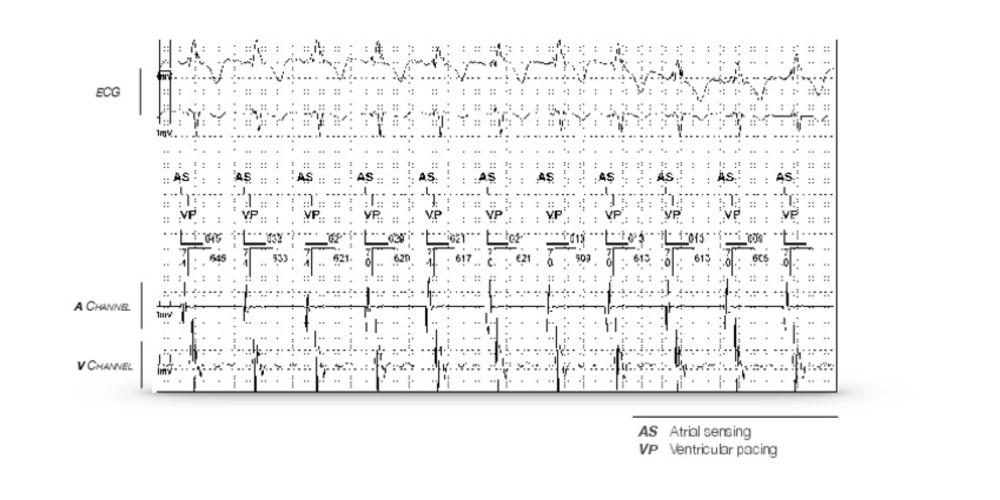
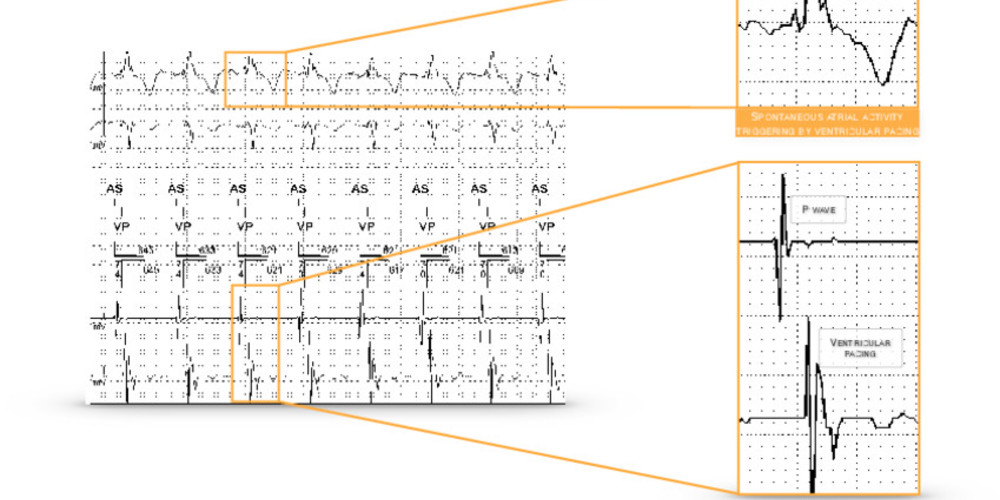
Graph and trace
Succession of AS-VP cycles (atrial sensing followed by ventricular pacing); this may therefore consist of a dual-chamber VDD or DDD mode that allows ventricular triggering (ventricular pacing) upon atrial sensing, which is impossible for VDI and DDI modes.
Other articles that may be of interest to you





The choice of pacing mode is the first essential step in programming a dual-chamber pacemaker since it directly affects the other remaining parameters to be programmed. Different pacing modes are programmable depending on the number of leads and the implanted device model. Pacing modes are defined by a 4-letter code describing their basic operation. The first letter defines the pacing chamber(s): ventricle (V), atrium (A), both (D) or none (O). The second letter defines the sensing chamber(s): same letters. The third letter indicates the mode of operation: inhibited (I), triggered (T), dual (D, I + T) or none (O). The fourth letter indicates whether there is rate modulation (rate response, R).
This tracing can correspond to the operation of VDD mode or DDD mode.
The VDD mode can be programmed on a dual-chamber pacemaker but can also be obtained from a single-chamber device with a single VDD lead bearing two floating atrial electrodes providing atrial sensing and two ventricular pacing/sensing electrodes. Sensing is carried out in both the atrium and the ventricle whereas pacing is only carried out in the ventricle; any atrial pacing is thus impossible. When the atrial rate is greater than the programmed minimum rate, the ventricle is paced synchronously up to the maximum synchronous rate. When the atrial rate is below the programmed minimum rate, the pacemaker operates in a pseudo-VVI mode. This mode is therefore acceptable in the absence of sinus dysfunction, and it is preferable to program a low minimum rate, possibly with rate hysteresis in order to preserve atrioventricular synchrony.
The advantages of single-lead VDD systems are: 1) only one lead is needed therefore enabling a sometimes shorter implantation procedure as well as a reduced amount of endovascular material; 2) the absence of trauma to the atrial wall allows preventing the development of atrial fibrosis; 3) in patients without sinus dysfunction, the physiological atrioventricular activation sequence is ensured. The drawbacks of single-lead VDD systems are: 1) that atrial sensing is sometimes less accurate than with a separate atrial lead, since the atrial dipole may move away from the chamber wall, especially during deep breathing and heart movements; 2) the detection of atrial arrhythmias is sometimes less accurate for the same reasons, rendering memory data less reliable; 3) in case of loss of paroxysmal atrial sensing during exertion and presence of atrioventricular block, the pacing rate returns to the base rate with possible sudden drop in rate, possible pacemaker syndrome and risk of pacemaker-mediated tachycardia; 4) this mode should be avoided in the presence of sinus dysfunction. The preferential indication of the VDD mode is therefore complete atrioventricular block with normal sinus function.
The basic principle of the DDD mode is to synchronize ventricular pacing on both atrial sensing and pacing. Any atrial sensing outside the refractory period and any atrial pacing results in ventricular pacing at the end of the AV delay in the absence of intrinsic ventricular sensing. This mode therefore preserves atrioventricular synchrony for low sinus rates and up to high rates (maximum rate limit).
In this patient, programming the VDD and DDD modes leads to the repetition of AS-VP sequences in spite of the presence of preserved atrioventricular conduction. One of the priorities of the programming is to avoid unnecessary right ventricular pacing in order to reduce battery consumption and prolong the life of the device but also to avoid the deleterious effect on heart function associated with right ventricular pacing. A high percentage of ventricular pacing in a patient with preserved atrioventricular conduction should warrant discussing the use of specific algorithms specifically designed to reduce the percentage of unnecessary ventricular pacing.