Pacemaker-mediated tachycardia due to loss of atrial capture
Tracing
Manufacturer Medtronic
Device PM
Field Refractory periods, PMT
N° 20
Patient
71-year-old patient implanted with a Kappa dual-chamber pacemaker for symptomatic long PR; routine consultation; the patient experiences dyspnea and frequent palpitations at rest.
Graph and trace
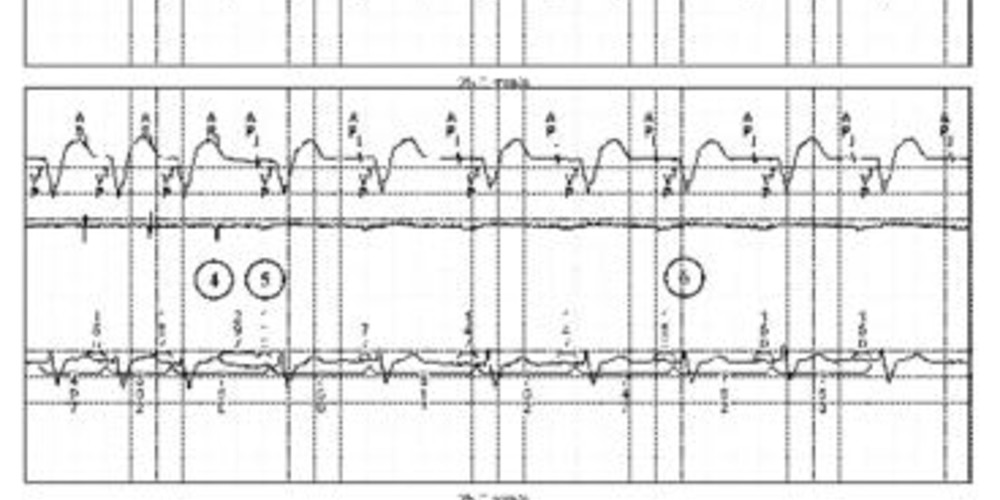
The first line corresponds to lead I with the superimposed markers, the second line to the atrial EGM and the last line to lead III with the superimposed intervals;
- repetition of AP-VP-AR intervals; the atrial EGM reveals the absence of atrial capture; ventricular capture is effective and is followed by atrial retrograde conduction; this conduction time is relatively short and atrial activity is sensed in the refractory period and therefore does not induce AV delay or ventricular pacing;
- occurrence of a possible atrial extrasystole or sinus activity, the VP-AR delay being shorter; it is also possible that the same retrograde atrial activity is sensed earlier (variable sensing delay time as a function of respiration for example);
- on this beat, the delay between VP and atrial sensing is prolonged; the atrial activity is no longer in the refractory period, is labeled AS, induces an AV delay and ventricular pacing;
- triggering of a PMT; the tachycardia rate (120 beats/minute) signifies that the retrograde conduction is slowed down comparatively to the beginning of the tracing; the atrial activities are no longer in the refractory period; the tachycardia rate is slower than the maximal tracking rate and corresponds to the sum of AV delay + retrograde conduction delay;
- triggering of the PMT interruption algorithm; prolongation of the refractory period on a beat; retrograde atrial activity falls within this refractory period;
- atrioventricular pacing with short AV delay (NCAP functioning); the EGM shows the absence of capture and retrograde conduction; the EGM allows eliminating sinus or atrial tachycardia, this atrial activity being directly related to the occurrence of the previous VP;
- new PMT; note that the interruption algorithm only restarts after 90 seconds explaining the persistence of the tachycardia.
Other articles that may be of interest to you





This tracing allows emphasizing an essential point in the management of patients with PMT. While it is highly important to program the interruption algorithm of these PMTs, it is imperative to also rectify the cause initiating the PMT. The best treatment for PMTs is prevention. The following events can promote AV dissociation, retrograde conduction and triggering of a PMT: ventricular extrasystole (most common cause), atrial extrasystole with increased AV delay in order to meet the programmed maximal tracking heart rate, AV delay programmed too long (the nodo-Hisian pathway has exited from its refractory period at the time of ventricular pacing), external or myopotential interference sensed by the atrial chain, lack of sensing or atrial pacing, absence of PVARP prolongation after removal of a magnet, application and removal of a magnet, programming the VDD mode in a patient with a sinus rhythm that is slower than the programmed minimum rate.
In this patient, the main issue is the loss of atrial capture. An increase in the amplitude of atrial pacing with sufficient margin allowed solving the problem.
A programming option may also be considered in this patient with complete atrioventricular block and sinus dysfunction: if, despite the programming modifications, there is persisting occurrence of PMTs, a programming in DDIR mode would enable an atrial and ventricular pacing, a rate response and would permanently prevent PMTs (an atrial sensing in DDI mode does not trigger AV delay or ventricular pacing).