Basic concepts
The main objectives of programming the basic settings of cardiac resynchronization therapy (CRT) are a) the maintenance of consistent BiV capture, and b) the optimization of hemodynamic function. CRT recipients suffer from a variety of underlying diseases. Therefore, the optimization of CRT must be tailored to each patient’s characteristics, as well as take into account the detection and treatment of ventricular tachyarrhythmia.
Minimal rate and pacing mode
Setting the basic pacing interval influences the percentage of atrial pacing. The left atrium is the only cardiac chamber that cannot be paced directly with a standard CRT system, although, in failing hearts, the left atrium plays a major role in determining the LV preload. The activation of the left atrium seems generally longer during atrial pacing (atrial latency + inter-atrial delay) than during sinus rhythm. As a consequence, the LV filling time may be shortened during atrial pacing.
In absence of sinus node dysfunction (SND), the basic heart rate (HR) should be kept slow in order to limit the percentage of atrial pacing as much as possible and to preserve the physiological activation of the left atrium and spare the battery. While both the VDD and DDD pacing modes can be programmed, the DDI mode should be avoided in absence of SND. In presence of SND at rest, whether endogenous or drug-induced, atrial pacing is mandatory. The DDD mode with rate response is preferred (in case of chronotropic incompetence) and the VDD mode must be avoided.
While there is no consensus regarding a minimal HR applicable to all patients, a basic pacing rate of 60 bpm is probably associated with a higher cardiac output than a rate of 40 bpm, without increasing the myocardial oxygen consumption. A resting HR >70 bpm should be avoided, although in presence of frequent ventricular extrasystoles or slow VT, an increase in the minimal HR may alleviate the arrhythmic burden and increase the BiV stimulation rate. However, these effects are usually temporary or only partially effective. One can also program algorithms to lower the incidence of atrial fibrillation (AF) by increasing the HR and forcing atrial stimulation. The benefits conferred by these measures in recipients of CRT systems remain to be shown.
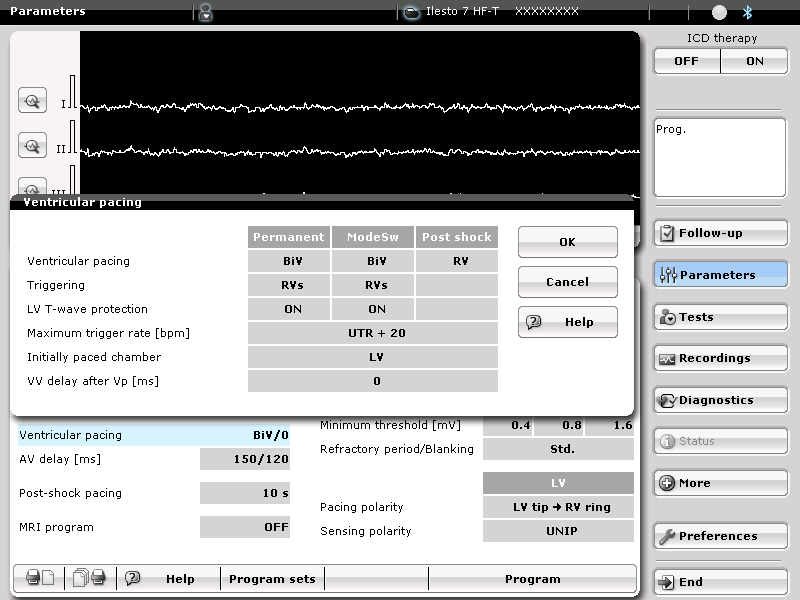
Algorithms have been developed by the device manufacturers to limit the percentage of ventricular stimulation, which is the inverse of the effect sought by resynchronization. It may be useful, however, when BiV stimulation needs to be interrupted, in case of lead dislodgement or in patients worsened by resynchronization. This kind of algorithm is programmable in CRT devices made by Microport CRM-Sorin (Safe-R) or Abbott (VIP), though not by Biotronik (Vp suppression will be available in future devices), Medtronic (MVP) or Boston Scientific (Rythmiq).
Upper tracking rate
The detailed characteristics of the upper tracking rate will be discussed in the paragraph dedicated to the programing during exercise. A large proportion of CRT system recipients are in sinus rhythm, with normal AV conduction and normal chronotropic response. Therefore, the upper tracking rate should be programmed just above the maximum sinus rate reached during exercise, thereby preserving BiV stimulation throughout exercise and preventing the development of Wenckebach periodicity. The programing of a slow upper tracking rate in CRT system recipients is a common error, which causes the loss of BiV stimulation at peak exercise, when it is probably most needed. The reliability of mode switches currently available in pacemakers is high enough to eliminate the risk of rapid pacing during atrial fibrillation. Therefore, it is safe to set the upper tracking rate as high as 150 bpm in many patients, particularly if a loss of BiV stimulation is observed during exercise.
Rate responsive mode
The principles of the rate responsive algorithm are detailed in the chapter dedicated to the programming of CRT during exercise. Spontaneous as well as drug-induced chronotropic insufficiency is often observed in patients suffering from heart failure. The programming of a rate responsive function in these cases increases the patient’s exercise capacity and improves the quality of life. The DDDR pacing mode should be favored in patients whose heart rate at peak exercise is <70% of the maximum predicted. In contrast, in presence of a normal chronotropic function, a rate responsive algorithm should be avoided, as it may unnecessarily increase the atrial pacing rate, increase myocardial oxygen consumption, and disturb hemodynamic function.
Mode switch
Patients suffering from heart failure are at high risk of developing episodes of atrial fibrillation. Therefore, a mode switch function should be systematically programmed. If the patient is in atrial fibrillation, a slightly increased resting heart rate (70 bpm for example) along with rate responsiveness, increases the percentage of BiV stimulation.
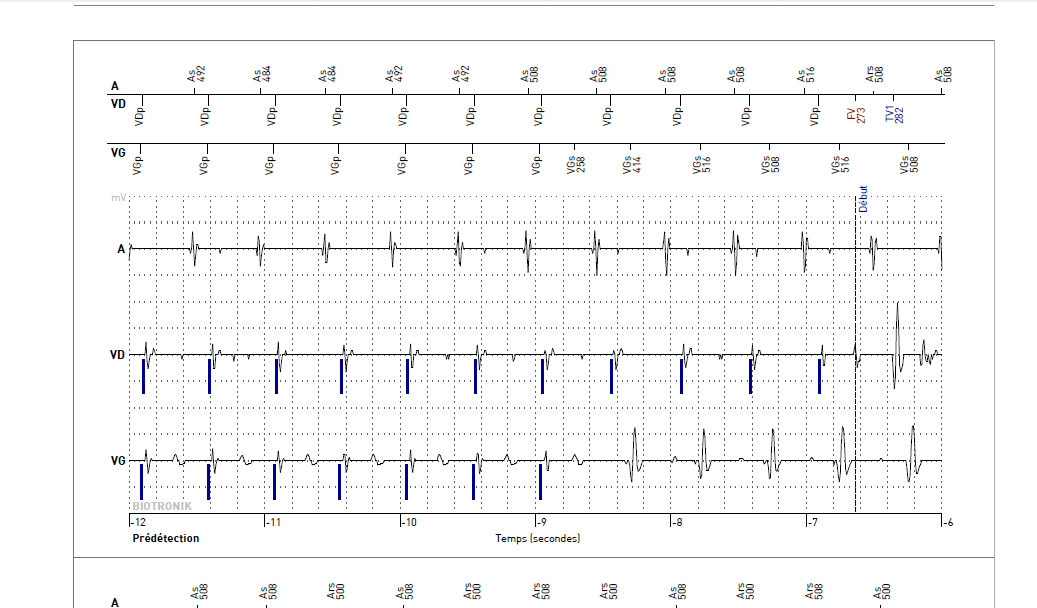
Atrial and ventricular sensing
The main objective of device programming is to obtain a percentage of BiV stimulation approaching 100%. Therefore, any ventricular oversensing inhibiting BiV stimulation must be thoroughly eliminated. Ventricular sensing must be programmed to avoid P and T waves sensing, as well as ventricular double counting, which is common in these patients in whom conduction disorders are prominent, while preserving reliable sensing of the ventricular electrograms, a key to the flawless function of a defibrillator.
The defibrillators made by Medtronic allow a choice between standard and integrated bipolar sensing if the implanted lead is a standard bipolar lead. Atrial undersensing may also lower the percentage of BiV stimulation. Exercise and an increase in respiratory motion are often the cause of unreliable atrial sensing. Therefore, a wider safety margin must be programmed than for sensing under resting conditions.
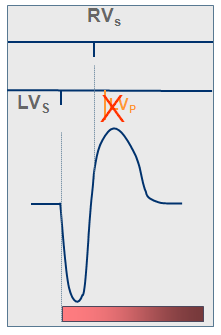
LV sensing in a defibrillator
LV sensing is not available with the Medtronic, Abbott and Microport CRM-Sorin defibrillators.