Medtronic Sensing and Detecting episodes
In this article
- SENSING AND DETECTING EPISODES
Auto-adjusting sensitivity
- DETECTION ZONES
- DETECTION COUNTERS
VT Counter
VF Counter
FVT Counter
Combine Counter
Auto-adjusting sensitivity
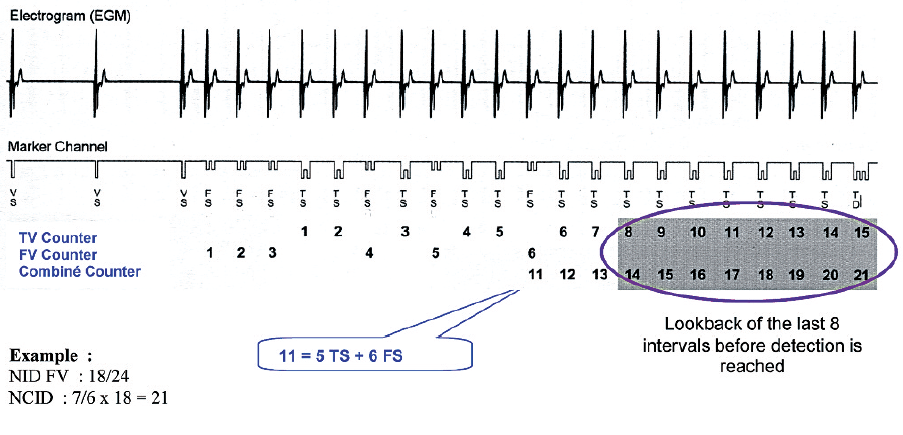
The effective operation of an Implantable Cardioverter Defibrillator (ICD) relies on its ability to detect both fast ventricular signals and low amplitude ventricular fibrillation signals without detecting T waves or extra-cardiac signals when the patient is in sinus rhythm. In order to ensure appropriate sensing, the device should be programmed with a high sensitivity (low detection threshold) and short refractory periods. Unlike a pacemaker the detection threshold is not programmed to a fixed value. The detection threshold automatically adjusts based on the amplitude of the preceding R-wave. Following a sensed or paced ventricular event the detection circuit starts a blanking period. The blanking period is short to avoid over detecting extended depolarization while still having the ability to detect a very rapid tachycardia. At the end of blanking, the level of sensitivity adaptation starts at a percentage of the amplitude of the sensed R-wave and then decays gradually until it reaches the minimum value programmed. The starting value of auto-adjusting sensitivity and degree of decay is different for each device manufacturer. The minimum sensing threshold is nominally programmed to 0.3 mV with a post ventricular paced blanking period of 120 ms in Medtronic devices.. The programmed sensitivity is assessed during induction of ventricular fibrillation for defibrillation threshold testing. The sensitivity must be high enough to detect low amplitude ventricular fibrillation waves while the refractory periods must be short enough to sense fast ventricular signals without detecting T waves or extra-cardiac signals.
After a ventricular sensed event, the sensitivity starts at 75% of the peak EGM amplitude to a maximum of 8 x the programmed value.
After a ventricular paced event a blanking period of 120ms is started. After the blanking period the sensitivity is increased to 4.5 x the programmed value to a maximum value of 1.8 mV.
Setting appropriate detection zones in a defibrillator is an essential step in ICD programming. Modern defibrillators allow the programming of several arrhythmia detection zones. These zones are based on the R-R intervals detected to classify an event as tachycardia or fibrillation. Specific programming for discrimination and therapies is available in each zone. The programmed number of zones and detection interval should be based on patient history, documented arrhythmias and the indication for implantation of the device.
In secondary prevention patients with heart failure, the programming of the detection interval is based on the cycle length of the clinical ventricular tachycardia (VT). In general, the detection zone is programmed 20 beats per minute slower than the rate of the clinical VT. Anti-arrhythmic treatment started or increased dosage after implantation is likely to change the rate of the VT.
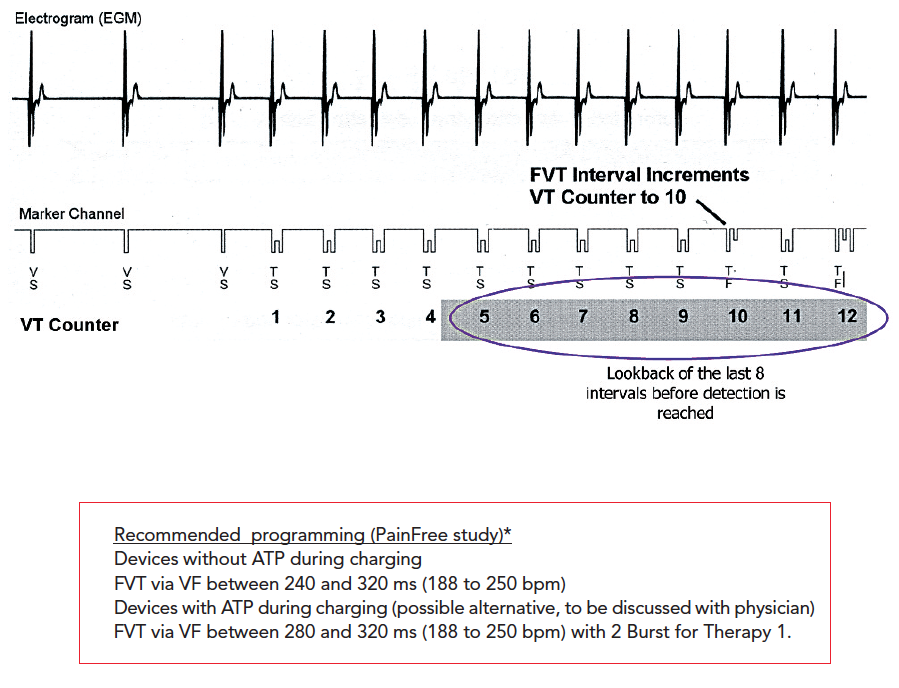
In primary prevention patients with heart failure, the risk of VT after device implantation is likely. Therefore the programming of two detection zones for the treatment of VT in addition to a zone for treatment of ventricular fibrillation (VF) is usually proposed. The purpose of programming separate zones is to specifically treat very rapid VT’s with anti-tachycardia pacing providing painless therapy compared to an electric shock. This has been demonstrated in clinical studies : PAIN FREE I and PAIN FREE II. These studies found that anti-tachycardia pacing avoids shocks 3 out of 4 times in fast VT’s (>188 bpm) without significantly increasing adverse events. This leads to a significant benefit in terms of quality of life. The results of this study justify the systematic programming of a sequence of anti-tachycardia pacing therapy in the fast ventricular tachycardia (FVT) detection zone.
In a patient with complete atrio-ventricular block the risk of inappropriate therapy for a supraventricular tachycardia is non-existent which enables programming of different detection zones without affecting the specificity. The use of discrimination algorithms isn’t helpful as any spontaneous tachycardia will be ventricular in origin.
Young and active patients : the risk of inappropriate treatment of atrial fibrillation or physiological acceleration in conduction must be considered when programming several detection and therapy zone. This can be achieved by programming detection zones that attempt to limit the overlap between normal physiological heart rates and the rate of clinical VT requiring therapy.
In a patient with Brugada syndrome the occurrence of regular, organized VT is extremely rare, whereas the risk of atrial fibrillation is high. Therefore programming a detection zone for the treatment of VT in addition to the VF zone is probably not beneficial and even dangerous. Programming a detection zone for monitoring alone can be used to detect potential arrhythmias with longer cycle lengths and assist in customizing programming. One detection zone for VF is usually programmed with a relatively high detection rate (often> 210-220 beats / min).
3 - DETECTION COUNTERSVT Counter
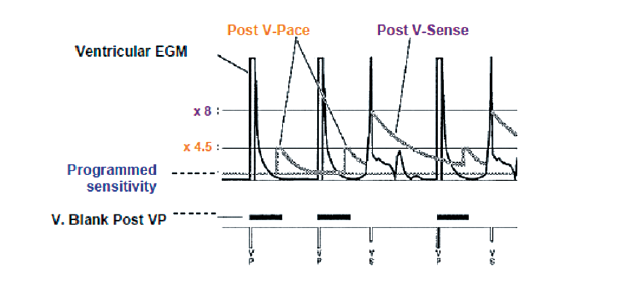
VT’s normally have a regular rhythm. In Medtronic devices, the VT zone uses a consecutive counter which sums the intervals falling within the VT detection zone until the number of intervals to detect (NID) is reached.
- An interval shorter than the VT detection interval => Counter + 1,
- An interval longer than VT detection interval => Counter reset to 0,
- An interval shorter than the VT and VF detection interval => Counter held. VF Counter
VF Counter
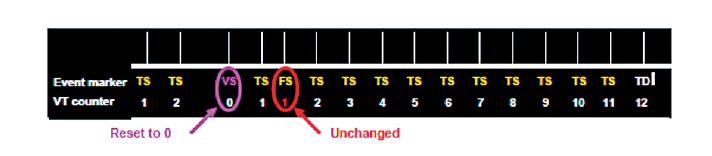
During VF, the intervals are short and irregular. They may have a low amplitude and become difficult to detect.
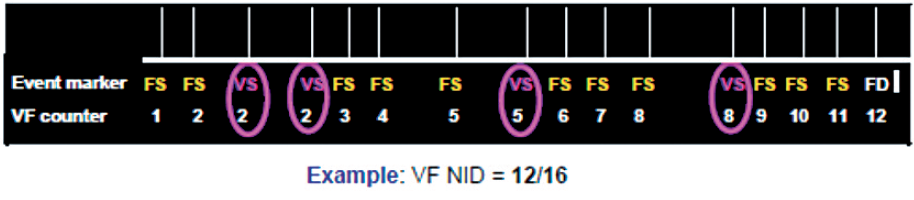
The VF detection counter sums the intervals in the VF zone among the last intervals : 9/12, 12/16, 18/24.
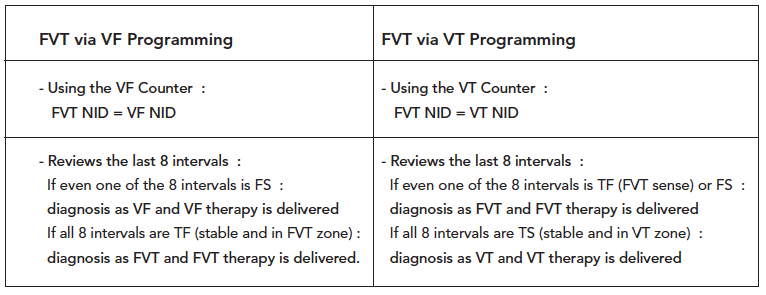
FVT Counter
Objective: to introduce a third detection area and a specific treatment program for FVT to initially treat the FVT as VT with anti tachycardia pacing rather than VF i.e. by shocks.
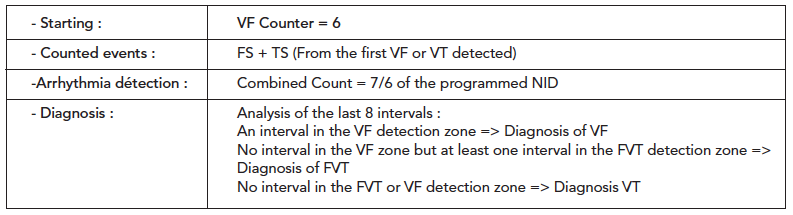
Combine Counter
Purpose:
Because the device counts VF and VT events separately, rhythms with variable cycle lengths can cause both event counters to increment during an episode. To prevent these rhythms from delaying detection, the device automatically enables the Combined Count.
Operating Details: