Basic concepts
One of the most common causes of oversensing and resultant inappropriate shocks is lead fracture. A systematic approach to the patient with suspected lead failure includes:
- a chest X-ray: radiographic abnormalities are not systematic and a conductor fracture can only be identified in less than half of the patients with ICD lead malfunctions.
- repeated measurement of high voltage and pacing impedances: last generation ICDs perform periodic measurement of pacing and high voltage impedance lead conductors. Daily automated assessment of the impedance of the high voltage electrodes using weak pulses are well correlated with values measured with full energy-shocks and may help detect a loss of lead integrity of the shock conductor before the occurrence of inappropriate or failed therapies. Out of range values or large abrupt changes in impedance are sensitive indicators of a lead fracture but in isolation are not sensitive enough for a timely detection of lead dysfunction. Indeed, some patients present with lead dysfunction by noting an abrupt variation in pacing or high voltage impedance without oversensing, but the other way is more frequent, i.e. repetitive oversensing without abnormal values of impedance.
- evaluation of sensing and pacing thresholds: alteration of the other standard lead parameters is often delayed and failure is poorly predicted by R-wave changes and/or changes in pacing threshold.
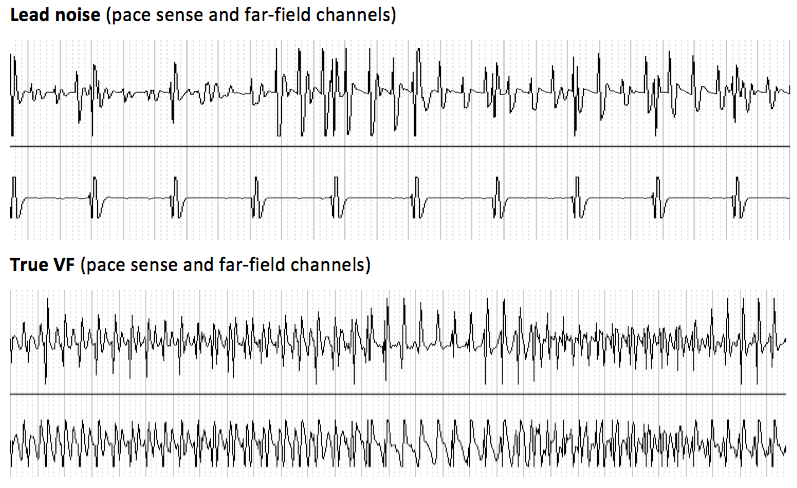
- analysis of the different stored electrograms: oversensing caused by lead fracture typically have suggestive but non-specific characteristics: intermittent sensing of sudden, non-physiological, high-frequency and high amplitude signals with possible saturation of the amplifiers and break-type electrogram abnormalities. Signals display substantial variability in amplitude or frequency, occur only during a small fraction of the cardiac cycles and may be positional. The rate of oversensed signals is frequently in the VF zone with intervals at the limit of the ventricular blanking period. These abnormal signals can affect the near field and/or the far field channels depending on the site of the fracture and may only become apparent after the delivery of a shock.
Loosened setscrew or header-connector problems (incomplete contact between the lead pin and header) have very similar presentations as a lead issue: lead impedance may be abnormally high and aspects of the oversensed electrograms can be similar. However, X-ray (magnified view directly over the pulse generator) may demonstrate an improper positioning of the pin connector in the header (pin coming out from the header). Moreover, connector problems tend to present acutely with a short interval from surgery to impedance rise or oversensing (within hours or days after the procedure) whereas lead failure usually manifest later except in cases of procedural damage. Manipulating the device inside the pocket may reproduce oversensing if there is a loose connection.
Other atypical situations may replicate the combination of abnormal impedance and/or oversensing of fast non physiological signals: header seal-plug problems with a specific aspect of sensed signals corresponding to the intervals between air bubbles escaping from the seal plug and lead to lead mechanical interaction (contact between the RV lead and an abandonned lead fragment or uncapped lead).
The differentiation between these different diagnoses to avoid overdiagnosis of lead fracture is sometimes difficult but may have important clinical implications since revision of the high voltage lead may not be requirred.