Basic concepts
ELECTRICAL SHOCKS IN VF ZONE
Defibrillators were originally developed to terminate life-threatening ventricular arrhythmias with an electrical shock. Cardioversion, which consists of delivering a low-energy shock synchronized to the upstroke of the R wave of an EGM, is distinguished from defibrillation, which consists of delivering a non-synchronized, high-energy shock. In the VF zone, synchronization of the shock may not be possible because of instability of the ventricular electrograms. In practice, defibrillators from the different manufacturers attempt to synchronize the shock to the R wave, including in the VF zone.
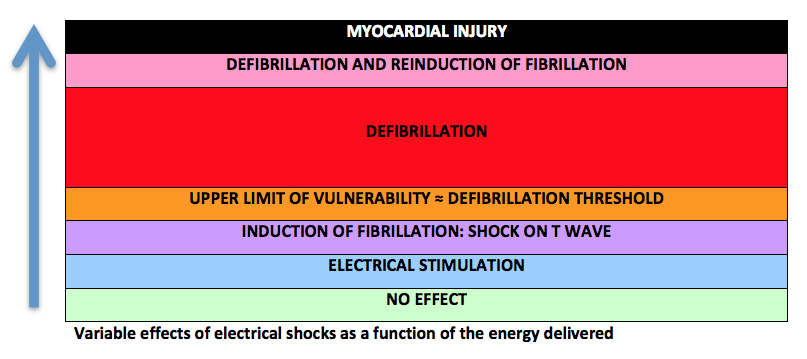
The effects of an electrical shock vary as a function of the energy delivered. Low energies, on the order of 1 J, delivered in the vulnerable period may induce an arrhythmia. The upper limit of vulnerability, a value correlated with the defibrillation threshold, is the lowest energy delivered in the ventricular vulnerable period that does not trigger VF. The probability of arrhythmia termination increases thereafter along an exponential curve as a function of the amplitude of the shock delivered, when synchronized with the R wave. Above a certain value, the risk of re-inducing an arrhythmia increases as well, thereby limiting the chances of therapeutic success. A shock of excessive amplitude may injure the myocardium.
The stored energy subsequently delivered by a defibrillator is expressed by the formula:
stored energy = ½ CV; where C = capacitance and V = voltage;
Various characteristics of the shock waveform, shock vector, shock amplitude and number of shocks delivered determine the success of defibrillation and may or may not be programmable.
Several variables pertaining to the shock waveform, its polarity, vector and amplitude, and the number of shocks delivered are programmable according to the manufacturers.
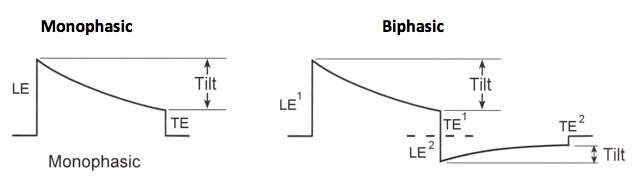
Shock waveform
After a long history of monophasic configuration, a biphasic shock waveform, which lowered the defibrillation threshold, was introduced. The first phase of a biphasic shock is equivalent to that of a monophasic shock, though with a lower critical mass; the second phase brings the membrane potential back to as near to zero as possible, in order to prevent the re-induction of VT or VF. The shock waveform can be programmed in some devices to be mono- or biphasic; however, the nominal waveform is always biphasic and should not be changed.
Shock polarity
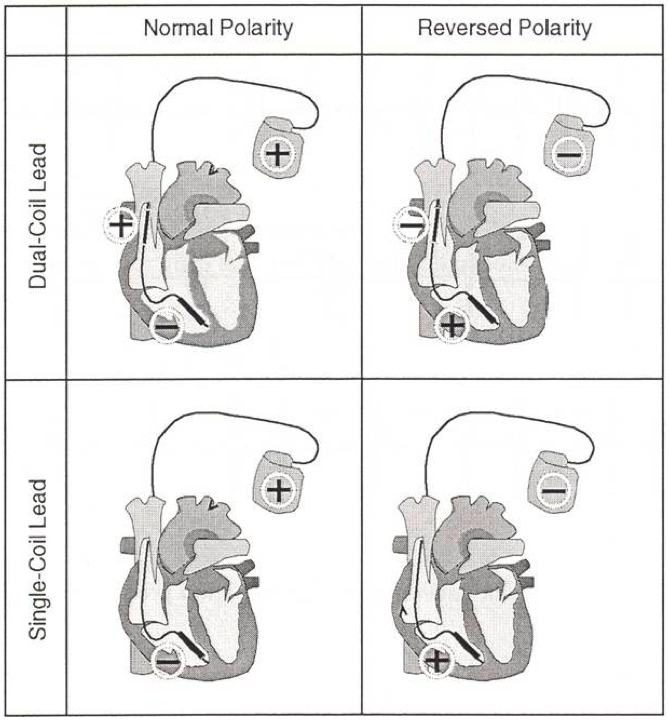
2 polarities are possible; an anodal shock corresponds at a shock with the right ventricular electrode as the anode in the first phase of a biphasic shock and as the cathode in the second phase; in contrast, a cathodal shock corresponds at a shock with the right ventricular electrode as the cathode in the first phase of a biphasic shock and as the anode in the second phase. The nominal polarity for the shocks of Medtronic, Abbott and Microport CRM-Sorin devices is anodal. In contrast, it is cathodal in Biotronik and Boston Science devices. The superiority of a given polarity (anodal versus cathodal) is still under debate, the probabilistic nature of defibrillation makes clinical studies comparing these 2 polarities very difficult to perform. Litterature suggests that the defibrillation thresholds may be lower with a right ventricular electrode used as an anode for the first phase of a biphasic shock, particularly when the DFT is high. According to specific manufacturer, the polarity may or may not be reversed during the delivery of a series of shocks.
Shock vector
The programming of this parameter depends on the number of shocking electrodes available. The defibrillation shock is delivered via a dedicated lead, which may be a single coil (one defibrillation electrode or coil placed inside the right ventricle), or a dual coil (one distal defibrillation electrode placed inside the right ventricle, and one more proximal defibrillation electrode placed in the superior vena cava) lead. Single coil shocks are delivered between the distal coil of the right ventricular lead and the can, while dual coil shocks are delivered between 1) the distal coil, 2) the proximal coil and 3) the pulse generator. With a dual coil electrode, the shock vector can be changed by including or excluding the proximal electrode in the superior vena cava or by excluding the pulse generator (cold can). The greater defibrillation efficacy contributed by a dual coil lead is currently debated. The orientation of the shock vector must cover the left ventricle uniformly; this vector depends on the position of the defibrillation coil(s) and of the pulse generator with respect to the heart. The distal right ventricular coil must be entirely contained inside the ventricular cavity, while the proximal coil of a dual-coil electrode must be placed high enough to prevent the dissipation of current at the level of the right atrial cavity. Placing the proximal coil inside the superior vena cava may be challenging. If it is floating inside the right atrium, it might be preferable to use the lead as a single coil.
Shock amplitude
In the VF zone, the strength of the first and subsequent shocks is usually programmed at the highest value the device is able to deliver. Programming of the defibrillation shock amplitude can be guided by the defibrillation threshold, defined as the least amount of energy that converts VF to sinus rhythm. According to the specific manufacturer, the amplitude corresponds to the delivered or the stored amount of energy.