Basic concepts
T-wave oversensing remains a significant problem in modern ICD systems and has been reported to occur in up to 8% of patients. It may cause inappropriate shock delivery during normal sinus rhythm particularly during exercise when both RT and TR intervals fulfill the VF detection rate. T-wave oversensing is usually divided into oversensing of the paced T-waves, oversensing of spontaneous T-waves in presence of an adequate R-wave and oversensing of spontaneous T-waves in presence of a small R-wave.
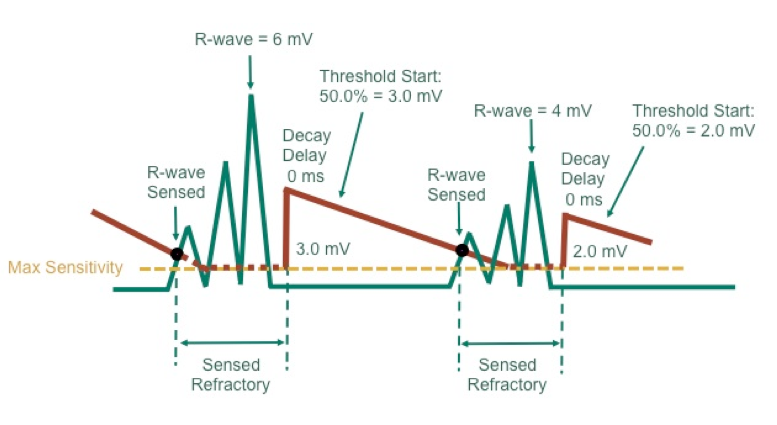
The requirements of the sensing circuitry of an ICD are different than those of a pacemaker since the need to detect rapid rhythms precludes the programming of long and fixed ventricular blanking periods, the need to detect fast, polymorphic, low-amplitude signals precludes programming low and fixed sensitivity, with the concomitant need to ignore T-waves.
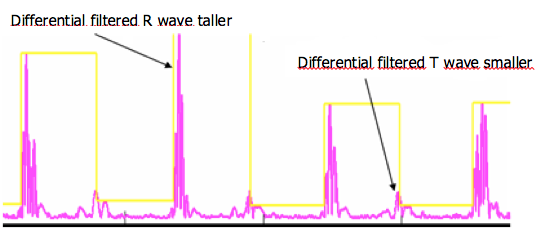
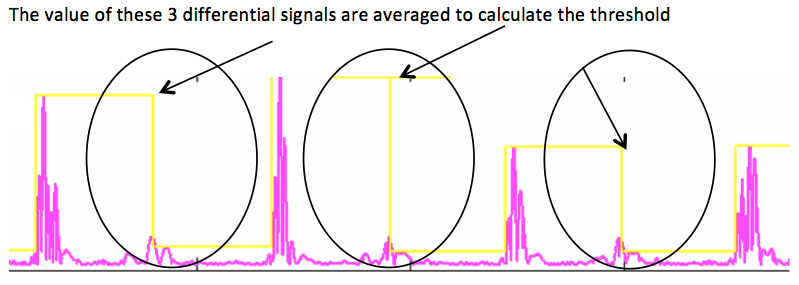
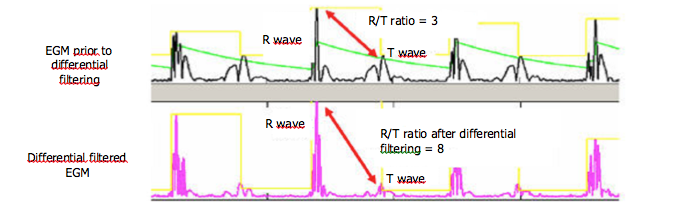
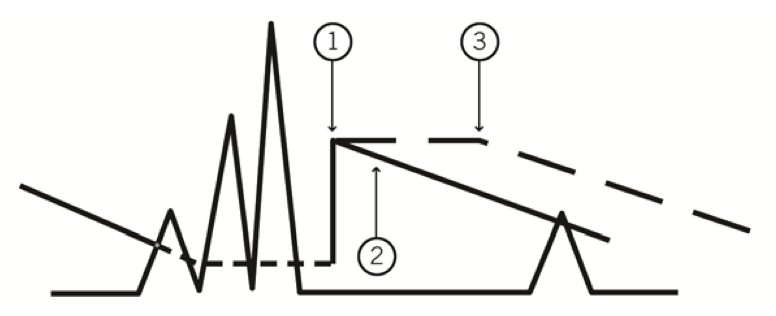
The crucial step to minimize T-wave oversensing is the choice of the range of bandpass filters by the manufacturers (difference between the high and low pass filters). The slew-rate of the T-wave (smooth signals) is less than that of the R-wave (sharp signals), with a usual frequency less than 5 Hz, but may change with use of drugs, ischemia, sympathetic tone or metabolic abnormalities. In some situations, the filters and the sensing amplifiers may not provide a large enough absolute difference between the R-wave amplitude and the T-wave amplitude. The amplitude of the T-wave may exceed the auto-adjusting threshold leading to T-wave oversensing.
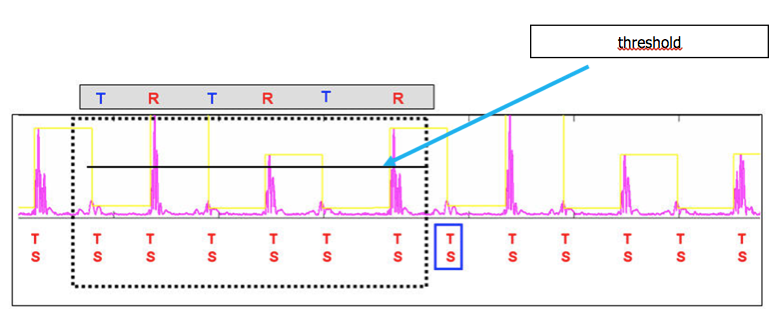
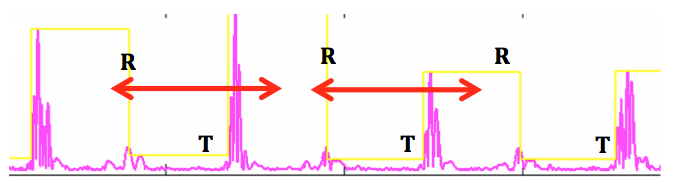
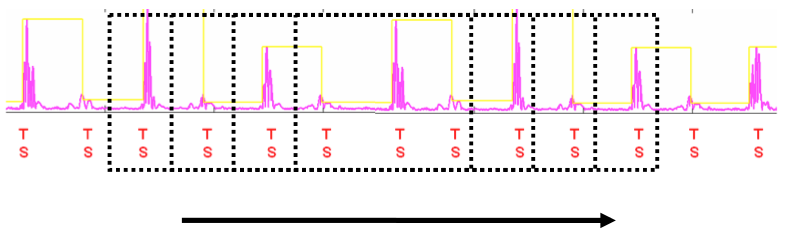
T-wave oversensing is associated with a typical aspect of alternating high-frequency (R-wave) and low-frequency (T-wave) signals on the near-field electrogram. The device counts the T-wave as an additional ventricular event doubling the measured ventricular rate. The magnitude of the alternation in intervals may also be important at low heart rate with a short QT interval (short RT and longer TR interval) but may be smaller especially during tachycardia and/or if the QT is prolonged (RT and TR nearly equivalent).
Three electrical patterns can lead to oversensing of the T wave after spontaneous beats:
- Delayed T-wave: it is likely to be observed in patients with long QT syndrome in whom repolarization is delayed when the ventricular sensitivity is at maximal level. Moreover, in these channelopathies, the QT interval, the morphology and amplitude of the T-wave can be modified dynamically increasing the risks of inappropriate therapies during exercise.
- High amplitude T-wave and adequate R-voltage: this can be observed in hypertrophic cardiomyopathy, short QT syndrome resulting in tall Q-wave, some forms of long QT syndrome, electrolyte abnormalities (hyperkalemia, hyperglycemia) and some uncommon but reversible causes of repolarization changes like alcohol intoxication.
- Small R-wave: when the R wave is of low voltage, oversensing of the T-wave becomes more likely to occur since the sensing threshold is automatically adapted to the R-wave amplitude and decreases over time. As a result, the device rapidly reaches high levels of sensitivity earlier in the cardiac cycle. Rapid deterioration of the amplitude of the R wave after implantation can be a manifestation of lead microdislodgement. Low R-wave amplitude can also be observed in patients with arrhythmogenic right ventricular cardiomyopathy, Brugada Syndrome, cardiac sarcoidosis, dilated cardiomyopathy involving the right ventricular chamber and can be a sign of disease progression.
In a limited proportion of cases, T-wave oversensing can be avoided by eliminating reversible causes. Large and/or delayed T waves can be corrected by reprogramming (variable possibilities according to different manufacturers) whereas the reprogramming options are limited in case of low-voltage R-wave and lead revision is often necessary.
To noninvasively manage T-waves oversensing, different options can be proposed: decreasing ventricular sensitivity to a less sensitive level (may be associated with undersensing of true VF particularly if the R-wave is small), lengthening the post-ventricular refractory period (most of the time ineffective), increasing the interval detection count or programming the tachycardia detection rate above twice the expected exercise-induced maximum heart rate (no impact on the occurrence of oversensing but decrease in the risk of inappropriate therapies). Administration of drugs like beta-blockers can be proposed to slow the heart rate.
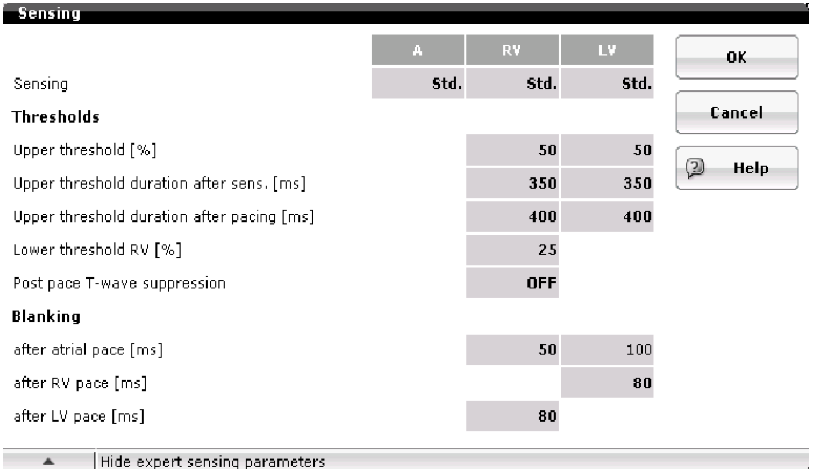
Some manufacturers (Biotronik and Abbott) provide other specific means to cover the T-wave signal: programmable threshold start, sensing decay delay and adjustable band pass filter for ventricular sensing.
The alternation of morphologies and/or intervals may be exploited to discriminate T-wave oversensing with a true VT using morphology and/or stability discriminators.
Medtronic has also developed a specific algorithm that withholds therapy when T wave oversensing is identified. The aim is not to prevent T-wave oversensing but to provide the appropriate diagnosis and to prevent the consequences.
Some of these programming features may compromise reliable sensing during VF. A revision of the system is required if the safety margin for sensing VF is insufficient (typically T-wave oversensing with low-voltage R-wave). Manufacturer-related differences in lead design and device-based signal processing and possible manufacturer specific lead/generator compatibility may explain why in clinical practice, the rate of T-wave oversensing seems to be different from one manufacturer to another without definitive testing from large, randomized studies. In some situations, a change of device manufacturer can be proposed with in some cases, resilution of the problem.
T-wave oversensing may be RV site-specific and if a new lead is implanted, the operator will try to relocate the electrode to a position with an R wave of greater amplitude and an increased R/T ratio. In infrequent situations, none of the RV sites provides acceptable signals (severe arrhythmogenic right ventricular cardiomyopathy) and surgical positioning of the high-voltage lead on the left ventricle has been performed.